Home > Clincal depts. > Department of Diagnostic Radiology (Interventional Radiology Center)
Department of Diagnostic Radiology (Interventional Radiology Center)
Masahiko Kusumoto, Miyuki Sone, Yasunori Mizuguchi, Gen Iinuma, Nachiko Uchiyama, Hirokazu Watanabe, Mototaka Miyake, Shunsuke Sugawara, Kimiteru Ito, Yuko Kubo, Chihiro Ito, Miyako Morooka, Nao Kikkawa, Shintaro Kimura, Yuta Maruki, Sawako Kaku, Junji Omori, Mizuki Ozawa, Yuji Koretsune
Introduction
The Department of Diagnostic Radiology provides a wide range of modalities, including interventional radiology (IR), general radiology, computed tomography (CT), magnetic resonance imaging (MRI), ultrasound, mammography, and nuclear medicine (Table 1).
In 2014, we launched the Interventional Radiology Center to facilitate widespread proliferation of IR in Japan and to provide various IR treatments for patients referred from other hospitals or clinics.
We seek individuals with outstanding leadership capabilities, proven academic and administrative experience, a vision to build and sustain programs at the forefront of imaging research, and a commitment to clinical experience.
Table 1. Number of Examinations per Modality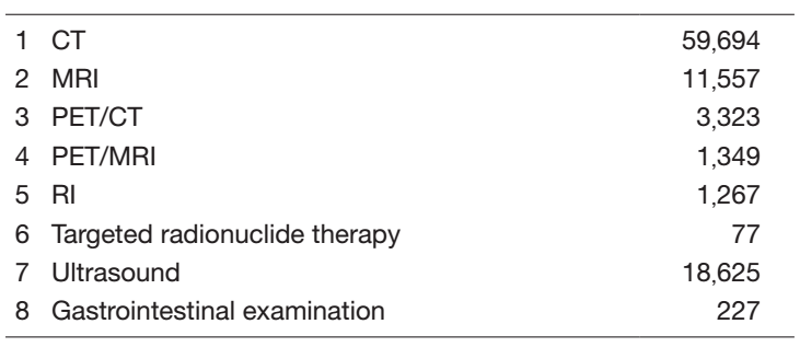
The team and what we do
In 2021, a total of 16 board-certified radiologists, two physicians and one ultrasound physician performed routine radiological diagnosis including IR procedures. We provided a total of 96,119 radiological diagnoses, the details of which are shown in Table 1. A total of 6,850 IR procedures were performed from April 2021 to March 2022 at the center (Table 2). Furthermore, we had several consultation phone calls regarding indications for various IR procedures from all over the country.
Table 2. Type of Percutaneous Interventional Radiology Procedure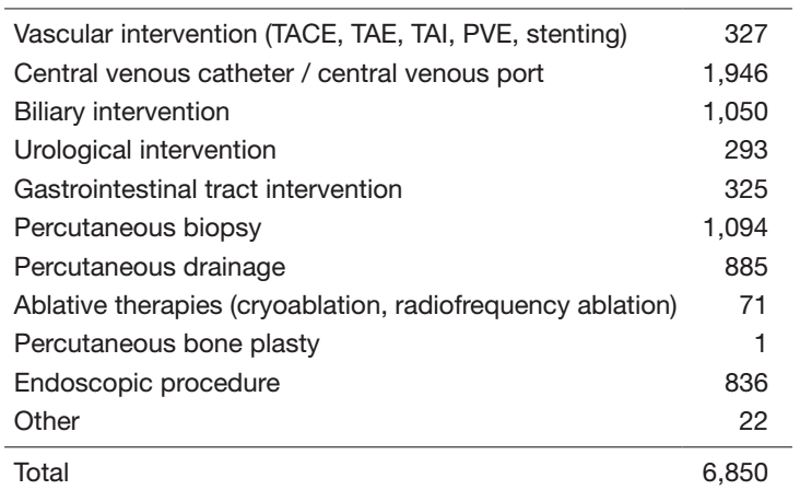
Research activities
The CT colonography (CTC) has been successfully introduced as an effective option for preoperative staging and colorectal screening in our center. Nearly 1,000 patients and/or candidates were examined with this modality in 2021. For the preparation for screening CTC, electronic cleansing with fecal barium tagging and automated CO2 gas insufflation systems have been established in formal National Cancer Center (NCC) collaboration studies with associated companies. Furthermore, we are now developing computer-aided detection (CAD) for colorectal lesions, especially for flat lesions. The main purpose of our CTC research work is to conduct a multicenter trial to establish evidence regarding fully digitalized CTC for a colorectal screening system in Japan.
A multi tracer consisting of F-18 FDG, and Cu-64 ATSM PET/CT imaging has been studied for cancer patients to improve the sensitivity and specificity of detecting tumor sites or tumor characteristics for treatment. F-18 FDG PET allows us to calculate the glucose metabolic rate of the tumor site and to predict the treatment response in patients treated with immune checkpoint inhibitors. Cu-64 ATSM PET/CT has been conducted in over 12 patients with brain tumor through the clinical research. Production of a new nuclide, Zr-89, will start by next year. The PET/MRI has been applied to more than 1000 cases of cancer patients per year and proved itself to be a powerful tool for managing malignancy. For cancer treatment using radioisotopes, internal radiotherapy was carried out with the use of radioactive iodine (I-131) chloride, Zevalin, Lutathera, Xofigo, and Raiatt.
Through the achievement of collaborative research with the associated company since 2009, digital breast tomosynthesis (DBT) has been introduced as an effective routine option for preoperative evaluation since March 2014. Up to March 2022, 5,507 patients were examined. Regarding image acquisition systems, a new software-based scatter correction enabling gridless imaging has been developed and acquired in clinical usage. Furthermore, new volumetric image reconstruction algorithms such as synthetic 2D, synthetic 3D, and thick slab images have been developed and evaluated to decrease radiation dose and the number of images for diagnosis.
In the project of "Public/Private R&D Investment Strategic Expansion PrograM (PRISM)", for the development of artificial intelligence to accelerate the creation of new drugs, we provided 2,000 chest CT images and diagnostic reports to build an integrated database for lung cancer treatment. We have also developed an annotation tool for radiological images in order to efficiently develop deep learning models.
A major departmental research theme is establishing an evidence base for interventional radiology (IR). We have conducted multi-institutional clinical trials as a steering organization as mentioned hereunder. The in-house research topics include: feasibility and efficacy of percutaneous needle biopsy for peritoneal masses, percutaneous gastrostomy for patients undergoing partial gastrectomy, and craniocaudal access to the superior sulcus lesions of the thorax. We have also developed novel IR techniques and software including palliative stent placement for the patients with multiple bowel obstructions, lymphatic embolization using a balloon, and a navigation system for vascular embolization and tumor ablation.
We have explored the efficacy of the ultra-high-resolution computed tomography (U-HRCT), which had been developed in the NCC. The research topics related to U-HRCT include: staging and evaluating the treatment efficacy of head and neck cancers; diagnostic accuracy of invasion to the pancreatic neural plexus in patients with pancreatic cancer, and simulation of IR procedures using the U-HRCT data. In addition, we have started developing radiomics and artificial intelligence for the detection and characterization of pancreatic tumor.
Clinical trials
We have led a multi-institutional cooperative study group of interventional radiology (JIVROSG: Japan Interventional Radiology in Oncology Study Group) since 2002 as a steering organization of 107 participating domestic institutions. A total of 29 studies had been completed and 22 were published. Currently, three clinical trials are ongoing.
In the nuclear medicine field, one clinical trial is ongoing: a phase I study evaluating the safety of Cu-64 ATSM for brain tumors. Also, we started developing another phase I study protocol of a new clinical trial evaluating the safety of Cu64 NCAB PET/CT for pancreas cancer.
Education
The clinical education and training of young radiologists is an important part of our department’s activities. Educational opportunities for domestic and overseas physicians have been provided. Due to the pandemic in 2021, in-person training for overseas trainees was precluded; however, we have continued online clinical conferences with Singapore General Hospital (Singapore), Institut Gustave Roussy (France) and the Dotter Institute (United States of America).
Future prospects
The Department of Diagnostic Radiology strives for excellence in clinical care, education, and research. Our goal is to provide outstanding patient-centered radiology services and to establish evidence in this area. Future challenges include promoting the active role of the Interventional Radiology Center opened in 2014 and facilitating imaging as biomarkers for personalized cancer treatments such as molecular-targeted agents for theranostics, immunotherapy, and boron neutron capture therapy.
The Interventional Radiology Center started extension work to create additional IR suites and a recovery room to facilitate improved access to oncologic interventions and better patient experiences. The center will be continuously aimed at (i) providing high-quality/high-speed clinical care with IR and procedures for patients both in and outside the hospital, (ii) promoting the education and training of IR procedures and clinical research for young physicians, and (iii) enhancing the usage and the accessibility of IR in the oncology field in Japan. Furthermore, we will collaborate on the MIRAI (Minimally-Invasive Revolutionary treatments with Advanced Intelligence) project in NCCH to develop innovative medical equipment and devices.
List of papers published
Journal
1. Nakamura S, Murakami N, Suzuki S, Ito K, Takemori M, Nakayama H, Kaga K, Chiba T, Iijima K, Takahashi K, Goka T, Itami J, Okamoto H, Igaki H. Monte Carlo simulation of tilted contact plaque brachytherapy placement for juxtapapillary retinoblastoma. Radiation oncology (London, England), 17:16, 2022
2. Kaku S, Motoi N, Watanabe H, Yoshida Y, Watanabe SI, Kusumoto M. “Real” Tumor-Spread Through Air Spaces of Lung Adenocarcinoma Presented Intrapulmonary Metastases Through Bronchiole Air Spaces: A Case Report. JTO clinical and research reports, 3:100273, 2022
3. Okubo Y, Kashima J, Teishikata T, Muraoka Y, Yotsukura M, Yoshida Y, Nakagawa K, Watanabe H, Kusumoto M, Watanabe SI, Yatabe Y. Prognostic Impact of the Histologic Lepidic Component in Pathologic Stage IA Adenocarcinoma. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer, 17:67-75, 2022
4. Sugawara H, Ito K, Watanabe H, Morita T, Yatabe Y, Watanabe SI, Kusumoto M. Clinical usefulness of PET/MRI in differentiating anterior mediastinal masses. Nuclear medicine communications, 43:92-99, 2022
5. Sugawara H, Watanabe H, Kunimatsu A, Abe O, Yatabe Y, Watanabe SI, Kusumoto M. Tumor size in patients with severe pulmonary emphysema might be underestimated on preoperative CT. European radiology, 32:163-173, 2022
6. Kitamura H, Hijioka S, Nagashio Y, Sugawara S, Nara S, Sone M, Esaki M, Arai Y, Okusaka T, Nakajima A. Use of endoscopic ultrasound-guided biliary drainage as a rescue of re-intervention after the placement of multiple metallic stents for malignant hilar biliary obstruction. Journal of hepato-biliary-pancreatic sciences, 29:404-414, 2022
7. Toki S, Sone M, Yoshida A, Nishisho T, Gokita T, Kobayashi E, Nakatani F, Chuman H, Sugawara S, Arai Y, Kawai A. Image-guided core needle biopsy for musculoskeletal lesions. Journal of orthopaedic science: official journal of the Japanese Orthopaedic Association, 27:448-455, 2022
8. Usui Y, Miura T, Kawaguchi T, Kosugi K, Uehara Y, Kato M, Kosugi T, Sone M, Nakamura N, Mizushima A, Miyashita M, Morita T, Yamaguchi T, Matsumoto Y, Satomi E. Palliative care physicians' recognition of patients after immune checkpoint inhibitors and immune-related adverse events. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer, 30:775-784, 2022
9. Sekine C, Uchiyama N, Watase C, Murata T, Shiino S, Jimbo K, Iwamoto E, Takayama S, Kurihara H, Satomi K, Yoshida M, Kinoshita T, Suto A. Preliminary experiences of PET/MRI in predicting complete response in patients with breast cancer treated with neoadjuvant chemotherapy. Molecular and clinical oncology, 16:50, 2022
10. Kitajima K, Watabe T, Nakajo M, Ishibashi M, Daisaki H, Soeda F, Tanemura A, Kanekura T, Yamazaki N, Ito K. Tumor response evaluation in patients with malignant melanoma undergoing immune checkpoint inhibitor therapy and prognosis prediction using 18F-FDG PET/CT: multicenter study for comparison of EORTC, PERCIST, and imPERCIST. Japanese journal of radiology, 40:75-85, 2022
11. Miyayama S, Arai Y, Matsui O. Transarterial chemoembolization for hepatocellular carcinoma with vascular invasion. The British journal of radiology, 20211316, 2022
12. Kawaguchi RK, Takahashi M, Miyake M, Kinoshita M, Takahashi S, Ichimura K, Hamamoto R, Narita Y, Sese J. Assessing Versatile Machine Learning Models for Glioma Radiogenomic Studies across Hospitals. Cancers, 13:2021
13. Takahashi S, Takahashi M, Tanaka S, Takayanagi S, Takami H, Yamazawa E, Nambu S, Miyake M, Satomi K, Ichimura K, Narita Y, Hamamoto R. A New Era of Neuro-Oncology Research Pioneered by Multi-Omics Analysis and Machine Learning. Biomolecules, 11:2021
14. Kobayashi K, Miyake M, Takahashi M, Hamamoto R. Observing deep radiomics for the classification of glioma grades. Scientific reports, 11:10942, 2021
15. Sugawara H, Watanabe H, Kunimatsu A, Abe O, Watanabe SI, Yatabe Y, Kusumoto M. Adenocarcinoma in situ and minimally invasive adenocarcinoma in lungs of smokers: image feature differences from those in lungs of non-smokers. BMC medical imaging, 21:172, 2021
16. Ito K, Kitajima K, Toriihara A, Ishibashi M, Nakahara T, Daisaki H, Ohe Y, Honda R, Kijima T, Hasegawa S, Nakajo M. 18F-FDG PET/CT for monitoring anti-PD-1 therapy in patients with non-small cell lung cancer using SUV harmonization of results obtained with various types of PET/CT scanners used at different centers. Annals of nuclear medicine, 35:1253-1263, 2021
17. Kubo Y, Ito K, Fujiwara Y, Yoshida T, Kusumoto M. Case Report: SAPHO Syndrome Mimicking Bone Metastases During Treatment With Pembrolizumab for Non-small Cell Lung Cancer. Frontiers in medicine, 8:679111, 2021
18. Sata M, Sasaki S, Oikado K, Saito Y, Tominaga J, Sakai F, Kato T, Iwasawa T, Kenmotsu H, Kusumoto M, Baba T, Endo M, Fujiwara Y, Sugiura H, Yanagawa N, Ito Y, Sakamoto T, Ohe Y, Kuwano K. Treatment and relapse of interstitial lung disease in nivolumab-treated patients with non-small cell lung cancer. Cancer science, 112:1506-1513, 2021
19. Saito Y, Sasaki S, Oikado K, Tominaga J, Sata M, Sakai F, Kato T, Iwasawa T, Kenmotsu H, Kusumoto M, Baba T, Endo M, Fujiwara Y, Sugiura H, Yanagawa N, Ito Y, Sakamoto T, Ohe Y, Kuwano K. Radiographic features and poor prognostic factors of interstitial lung disease with nivolumab for non-small cell lung cancer. Cancer science, 112:1495-1505, 2021
20. Sugawara S, Sone M, Itou C, Kimura S, Kusumoto M, Kato T, Yonemori K, Yatabe Y, Arai Y. Analysis of factors affecting the diagnostic yield of image-guided percutaneous core needle biopsy for peritoneal/omental lesions. Abdominal radiology (New York), 46:4499-4508, 2021
21. Kikkawa N, Ito K, Yoshida H, Kato MK, Kubo Y, Onishi Y, Sugawara H, Kato T, Kusumoto M. Magnetic resonance imaging findings in 11 cases of dedifferentiated endometrial carcinoma of the uterus. Japanese journal of radiology, 39:477-486, 2021
22. Ito Y, Maeshima AM, Hatta S, Saito Y, Fujino T, Makita S, Fukuhara S, Munakata W, Taniguchi H, Suzuki T, Maruyama D, Sone M, Izutsu K. Use of Core-Needle Biopsy for the Diagnosis of Malignant Lymphomas in Clinical Practice. Acta haematologica, 144:641-648, 2021
23. Koretsune Y, Sone M, Arai Y, Sugawara S, Itou C, Kimura S, Kusumoto M. Feasibility and Safety of the Craniocaudal Approach for Superior Sulcus Lesions of the Thorax. Cardiovascular and interventional radiology, 44:1456-1461, 2021
24. Itou C, Arai Y, Sone M, Sugawara S, Onishi Y, Kimura S. Transgastric Feeding Tube Insertion into the Jejunum after Esophagectomy: Direct Puncture of the Gastric Conduit. Journal of vascular and interventional radiology: JVIR, 32:1464-1469, 2021
25. Ozawa M, Yamamoto M, Yamada K, Sugawara T, Zako R, Suzuki A, Hitomi S, Hara T, Yamamoto K, Kondo H, Oba H. Intranodal Embolization for Groin Lymphocele. Interventional Radiology, 6:117-121, 2021
26. Ozawa M, Sone M, Arai Y, Sugawara S, Itou C, Kimura S, Okamoto D, Kusumoto M. Trans-Colostomy Placement of a Button Gastrostomy Tube for Malignant Bowel Obstruction in Patients with Peritoneal Carcinomatosis. The Arab Journal of Interventional Radiology, 5:106-109, 2021
27. Arai Y. A new window connecting medical oncologists and interventional oncologists. Japanese journal of clinical oncology, 51:1023, 2021
28. Arai Y. Interventional Radiology for Whom. Cardiovascular and interventional radiology, 44:633-634, 2021
29. Murakami R, Tani H, Kumita S, Uchiyama N. Diagnostic performance of digital breast tomosynthesis for predicting response to neoadjuvant systemic therapy in breast cancer patients: A comparison with magnetic resonance imaging, ultrasound, and full-field digital mammography. Acta radiologica open, 10:2.05846E+16, 2021
30. Kashihara T, Nakayama Y, Ito K, Kubo Y, Okuma K, Shima S, Nakamura S, Takahashi K, Inaba K, Murakami N, Igaki H, Ohe Y, Kusumoto M, Itami J. Usefulness of Simple Original Interstitial Lung Abnormality Scores for Predicting Radiation Pneumonitis Requiring Steroidal Treatment After Definitive Radiation Therapy for Patients With Locally Advanced Non-Small Cell Lung Cancer. Advances in radiation oncology, 6:100606, 2021