Home > Clincal depts. > Department of Palliative Medicine
Department of Palliative Medicine
Eriko Satomi, Koji Amano, Hiroto Ishiki, Daisuke Kiuchi, Akiko Abe, Yaeko Kobayashi, Yuma Takeda, Rebekah Kojima
Introduction
The palliative care service started with a palliative care team of multidisciplinary professionals (palliative care specialists, psycho-oncologists, certified nurses, pharmacists, psychologists, hospital play staff, acupuncturists) in the National Cancer Center Hospital (NCCH) in 1999 and the Department of Palliative Care and Psycho-Oncology was established in 2010 with the reorganization of the NCCH. In 2013, the Department of Palliative Medicine started.
The Team and What We Do
We provide palliative care to patients and their families as members of the palliative care team collaborating with primary doctors, nurses, and other professionals to create an individualized palliative care plan. Our goals are:
- Relieve pain and other physical symptoms
- Focus on patients’ emotional and spiritual concerns, and those of their caregivers
- Coordinate patients’ care
- Improve the quality of life of patients with cancer
- Advance care planning
Patient demography at the outpatient clinic and the palliative care team (Table 1)
Table 1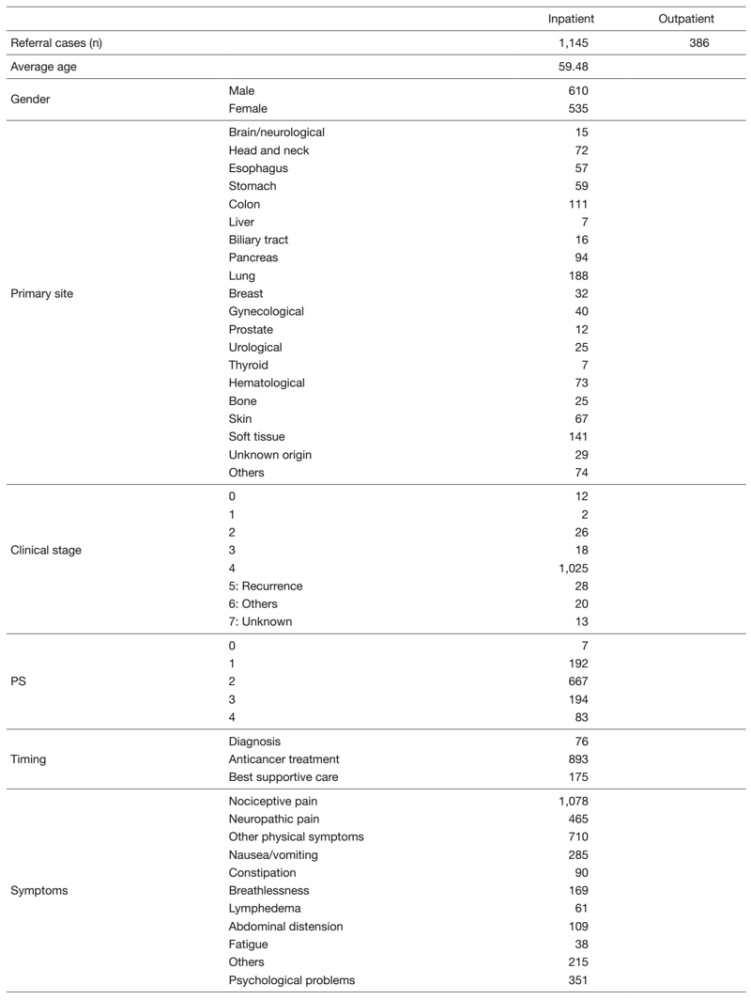
Research activities
We are participating in and conducting multicenter observational studies and interventional studies for supportive and palliative care, and continuously planning palliative care research for the innovation of palliative care.
Clinical trials
EASED (East-Asian collaborative Study to Elucidate the Dying process), JORTC-PAL16 (A Phase III, international, multi-center, double-blind, dose increment, parallel-arm, randomized controlled trial of duloxetine versus pregabalin over 14 days for opioid unresponsive cancer- related neuropathic pain), EORTC-QOL study (EORTC PATSAT-C33, EORTC OUT-PATSAT7, EORTC COMU26, Development of a module to supplement the EORTC Core instruments for assessment of Health Related Quality of Life in patients with Metastatic Breast Cancer (Phase I-III)), Development of measurement of eating-related distress etc.
Education
We have two training courses for doctors who will be palliative care specialists and for residents to learn primary palliative care. All the surgical and medical oncology residents in the NCCH need the knowledge and skills about primary supportive and palliative care in oncology. They participate in our team for four weeks and undergo on-the-job training for palliative medicine. A total of 18 residents finished the four-week palliative medicine course in 2021. They learned specialist palliative care in oncology including physical, psychosocial, and spiritual supportive care during anti-cancer therapy as well as end-of-life care, and support for patients’ decision making and advance care planning.
Future prospects
We will continue to provide qualified palliative cancer care with an integrated palliative care model in clinical practice throughout the continuum of a person’s disease, regardless of whether it is early or later in the course of the disease. In addition, we will enhance our palliative care education program for specialists and oncologists. We also continuously conduct high-level palliative care research in order to strengthen evidence to improve palliative care practice.
List of papers published
Journal
1. Tsubokura M, Adegawa Y, Kojima M, Tanosaki R, Ohtake R, Kase Y, Iwashita N, Kasane M, Nakabayashi S, Takeuchi S, Kato K, Boku N, Kanemitsu Y, Okusaka T, Fujimoto H, Yonemori K, Ishiki H, Kawamura K, Satomi E, Matsushita H. Adverse effects of cell-free and concentrated ascites reinfusion therapy for malignant ascites: a single-institute experience. BMC cancer, 22:268, 2022
2. Ishiki H, Hirayama T, Horiguchi S, Iida I, Kurimoto T, Asanabe M, Nakajima M, Sugisawa A, Mori A, Kojima Y, Udagawa R, Tsuchiya H, Oki M, Shimizu M, Yanai Y, Touma S, Nozawa K, Kojima R, Inamura N, Maehara A, Suzuki T, Satomi E. A Support System for Adolescent and Young Adult Patients with Cancer at a Comprehensive Cancer Center. JMA journal, 5:44-54, 2022
3. Hirayama T, Kojima R, Udagawa R, Yanai Y, Ogawa Y, Shindo A, Tanaka M, Kobayashi M, Ishiki H, Satomi E. A Questionnaire Survey on Adolescent and Young Adult Hiroba, a Peer Support System for Adolescent and Young Adult Cancer Patients at a Designated Cancer Center in Japan. Journal of adolescent and young adult oncology, 11:309-315, 2022
4. Matsuda Y, Yamaguchi T, Matsumoto Y, Ishiki H, Usui Y, Kako J, Suzuki K, Matsunuma R, Mori M, Watanabe H, Zenda S. Research policy in supportive care and palliative care for cancer dyspnea. Japanese journal of clinical oncology, 52:260-265, 2022
5. Hirayama T, Kojima R, Udagawa R, Yanai Y, Ogawa Y, Tanaka M, Kayano A, Mashiko Y, Ogata K, Ishiki H, Satomi E. A Hospital-Based Online Patients Support Program, Online Adolescent and Young Adult Hiroba, for Adolescent and Young Adult Cancer Patients at a Designated Cancer Center in Japan. Journal of adolescent and young adult oncology, 2022
6. Ueno T, Yatsuoka W, Ishiki H, Miyano K, Uezono Y. Effects of an oral mucosa protective formulation on chemotherapy- and/or radiotherapy-induced oral mucositis: a prospective study. BMC cancer, 22:90, 2022
7. Arraras JI, Giesinger J, Shamieh O, Bahar I, Koller M, Bredart A, Kuljanic K, Costantini A, Greimel E, Sztankay M, Wintner LM, Carreiro de Sousa M, Ishiki H, Kontogianni M, Wolan M, Kikawa Y, Lanceley A, Gioulbasanis I, Harle A, Kuliś D . Cancer patient satisfaction with health care professional communication: An international EORTC study. Psycho-oncology, 31:541-547, 2022
8. Kashihara T, Ishiki H, Kato K. Definitive Chemoradiotherapy for Older Patients With Esophageal Cancer. JAMA oncology, 8:304-305, 2022
9. Abe A, Amano K, Ishiki H. Prophylactic Scopolamine Butylbromide and Death Rattle in Patients at the End of Life. JAMA, 327:285, 2022
10. Hatano Y, Morita T, Mori M, Aoyama M, Yoshida S, Amano K, Terabayashi T, Oya K, Tsukuura H, Hiratsuka Y, Maeda I, Kizawa Y, Tsuneto S, Shima Y, Masukawa K, Miyashita M. Association between experiences of advanced cancer patients at the end of life and depression in their bereaved caregivers. Psycho-oncology, 2022
11. Alderman B, Allan L, Amano K, Bouleuc C, Davis M, Lister-Flynn S, Mukhopadhyay S, Davies A. Multinational Association of Supportive Care in Cancer (MASCC) expert opinion/guidance on the use of clinically assisted nutrition in patients with advanced cancer. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer, 30:2983-2992, 2022
12. Matsunuma R, Yamaguchi T, Mori M, Ikari T, Suzuki K, Matsuda Y, Matsumoto Y, Watanabe H, Amano K, Kamura R, Kizawa Y. Predictive Factors for the Development of Dyspnea Within 7 Days After Admission Among Terminally Ill Cancer Patients. The American journal of hospice & palliative care, 39:413-420, 2022
13. Usui Y, Miura T, Kawaguchi T, Kosugi K, Uehara Y, Kato M, Kosugi T, Sone M, Nakamura N, Mizushima A, Miyashita M, Morita T, Yamaguchi T, Matsumoto Y, Satomi E. Palliative care physicians' recognition of patients after immune checkpoint inhibitors and immune-related adverse events. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer, 30:775-784, 2022
14. Matsuoka H, Clark K, Fazekas B, Oyamada S, Brown L, Ishiki H, Matsuda Y, Hasuo H, Ariyoshi K, Lee J, Le B, Allcroft P, Kochovska S, Fujiwara N, Miyaji T, Lovell M, Agar M, Yamaguchi T, Satomi E, Iwase S, Phillips J, Koyama A, Currow DC. Phase III, international, multicentre, double-blind, dose increment, parallel-arm, randomised controlled trial of duloxetine versus pregabalin for opioid-unresponsive neuropathic cancer pain: a JORTC-PAL16 trial protocol. BMJ open, 12:e050182, 2022
15. Ito T, Yokomichi N, Ishiki H, Kawaguchi T, Masuda K, Tsukuura H, Funaki H, Suzuki K, Oya K, Nakagawa J, Mori M, Yamaguchi T. Optimal Paracentesis Volume for Terminally Ill Cancer Patients With Ascites. Journal of pain and symptom management, 62:968-977, 2021
16. Kosaka M, Honma Y, Ishiki H. Unresolved questions regarding the promise of the TPEx regimen. The Lancet. Oncology, 22:e227, 2021
17. Amano K, Satomi E, Oyamada S, Ishiki H, Sakashita A, Miura T, Maeda I, Hatano Y, Yamauchi T, Oya K, Nakagawa J, Hiratsuka Y, Hirohashi T, Morita T, Mori M, on behalf of the East-Asian collaborative cross-cultural Study to Elucidate the Dying process(EASED) investigators. The prevalence of artificially administered nutrition and hydration in different age groups among patients with advanced cancer admitted to palliative care units. Clinical Nutrition Open Science, 40:69-78, 2021
18. Arakawa S, Amano K, Oyamada S, Maeda I, Ishiki H, Miura T, Hatano Y, Naito AS, Sato M, Ito T, Kosugi K, Miyake S, Morita T, Mori M. Effects of parenteral nutrition and hydration on survival in advanced cancer patients with malignant bowel obstruction: secondary analysis of a multicenter prospective cohort study. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer, 29:7541-7549, 2021
19. Amano K, Ishiki H, Miura T, Maeda I, Hatano Y, Oyamada S, Yokomichi N, Tagami K, Odagiri T, Ito T, Baba M, Morita T, Mori M. C-Reactive Protein and Its Relationship with Pain in Patients with Advanced Cancer Cachexia: Secondary Cross-Sectional Analysis of a Multicenter Prospective Cohort Study. Palliative medicine reports, 2:122-131, 2021
20. Ishiki H, Hamano J, Nagaoka H, Matsuda Y, Tokoro A, Matsuoka H, Izumi H, Sakashita A, Kizawa Y, Oyamada S, Yamaguchi T, Iwase S. Prevalence of Extrapyramidal Symptoms in Cancer Patients Referred to Palliative Care: A Multicenter Observational Study (JORTC PAL12). The American journal of hospice & palliative care, 38:823-829, 2021
21. Iwaki M, Kessoku T, Kanamori T, Abe K, Takeno N, Kawahara R, Fujimoto T, Igarashi T, Kumakura Y, Suzuki N, Kamiya K, Suzuki N, Tagami K, Saeki T, Mawatari H, Sakurai H, Higashibata T, Hirohashi T, Nakajima A, Ichikawa Y, Ishiki H. Tapentadol Safety and Patient Characteristics Associated with Treatment Discontinuation in Cancer Therapy: A Retrospective Multicentre Study in Japan. Pain and therapy, 10:1635-1648, 2021
22. Ishiki H, Hasuo H, Matsuda Y, Matsuoka H, Hiramoto S, Higuchi M, Yoshida K, Tokoro A, Hatano Y, Hori T, Kinkawa J, Nojima M. Prevalence of myofascial pain syndrome and efficacy of trigger point injection in patients with incurable cancer. A multicenter, prospective observational study. (MyCar study). Pain medicine (Malden, Mass.), 2021
23. Yokoyama K, Ishiki H. Questions Regarding Patient-Reported Symptom Burden as a Predictor of Emergency Department Use and Unplanned Hospitalization in Head and Neck Cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology, 39:2415-2416, 2021
24. Kosaka M, Mizutani T, Ishiki H. What Is the Optimal Treatment for Vulnerable Older Women With Ovarian Cancer? JAMA oncology, 7:1725-1726, 2021
25. Amano K, Hopkinson J, Baracos V. Psychological symptoms of illness and emotional distress in advanced cancer cachexia. Current opinion in clinical nutrition and metabolic care, 2021
26. Yokota S, Amano K, Oyamada S, Ishiki H, Maeda I, Miura T, Hatano Y, Uneno Y, Hori T, Matsuda Y, Kohara H, Suzuki K, Morita T, Mori M, on behalf of the East-Asian collaborative cross-cultural Study to Elucidate the Dying process (EASED) investigators. Effects of artificial nutrition and hydration on survival in patients with head and neck cancer and esophageal cancer admitted to palliative care units. Clinical Nutrition Open Science, 41:33-43, 2021
27. Ikari T, Hiratsuka Y, Yamaguchi T, Mori M, Uneno Y, Taniyama T, Matsuda Y, Oya K, Amano K, Tagami K, Inoue A. Is the 1-day surprise question a useful screening tool for predicting prognosis in patients with advanced cancer?-a multicenter prospective observational study. Annals of palliative medicine, 10:11278-11287, 2021
28. Amano K, Kiuchi D, Ishiki H, Matsuoka H, Satomi E, Morita T. Clinical Implications of the Interdisciplinary Psychosocial Approach and Integrative Care for Patients with Advanced Cancer and Family Members in the Nutritional Support and Cancer Cachexia Clinic. DEN open, 16:147-152, 2021
29. Miura T, Elgersma R, Okizaki A, Inoue MK, Amano K, Mori M, Chitose H, Matsumoto Y, Jager-Wittenaar H, Ottery FD . A Japanese translation, cultural adaptation, and linguistic and content validity confirmation of the Scored Patient-Generated Subjective Global Assessment. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer, 29:7329-7338, 2021
30. Maeda I, Inoue S, Uemura K, Tanimukai H, Hatano Y, Yokomichi N, Amano K, Tagami K, Yoshiuchi K, Ogawa A, Iwase S. Low-Dose Trazodone for Delirium in Patients with Cancer Who Received Specialist Palliative Care: A Multicenter Prospective Study. Journal of palliative medicine, 24:914-918, 2021
2. Mori M, Fujimori M, Ishiki H, Nishi T, Hamano J, Otani H, Uneno Y, Oba A, Morita T, Uchitomi Y. Adding a Wider Range and "Hope for the Best, and Prepare for the Worst" Statement: Preferences of Patients with Cancer for Prognostic Communication. Oncologist, 24: e943-e952, 2019
3. Morita T, Kiuchi D, Ikenaga M, Abo H, Maeda S, Aoyama M, Shinjo T, Kizawa Y, Tsuneto S, Miyashita M. Difference in Opinions About Continuous Deep Sedation Among Cancer Patients, Bereaved Families, and Physicians. J Pain Symptom Manage, 57:e5-e9, 2019
4. Ishiki H, Yamaguchi T, Matsumoto Y, Kiuchi D, Satomi E. Effect of early palliative care: complex intervention and complex results. Lancet Oncol, 19:e221, 2018
5. Ishiki H, Kinkawa J, Watanabe A, Watanabe C, Chiba T, Yasui H, Shimada N, Ariyoshi K, Nojima M, Iwase S, Tojo A, Imai K. Prevalence of myofascial pain syndrome in patients with incurable cancer. J Bodyw Mov Ther, 22時32分8-332, 2018