HOME > Publication & Reports > Annual Report 2016 > Hospital East
Department of Thoracic Surgery
Masahiro Tsuboi, Tomoyuki Hishida, Keiju Aokage, Tomohiro Miyoshi, Keigo Sekihara, Masahito Naito, Junji Yoshida
Introduction
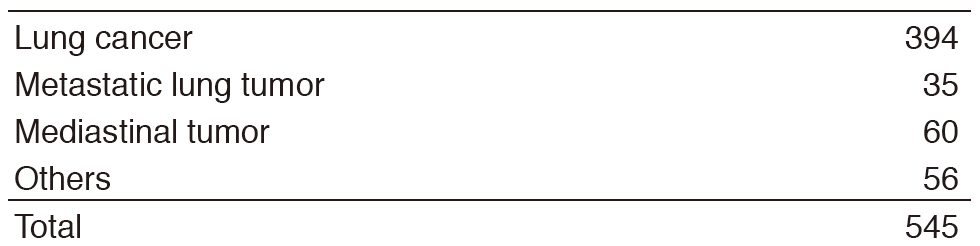
The Department of Thoracic Surgery has three missions: surgical treatment, surgical resident training, and clinical research. Thoracic surgeries involve the treatment of thoracic neoplasms, primary and metastatic lung tumors, as well as mediastinal, pleural, and chest wall tumors. Our department specializes in the surgical treatment of pulmonary carcinomas. Routine surgical treatment modalities for carcinomas include limited resection (wedge or segmental resection) and simple resection (lobectomy or pneumonectomy) with or without systematic lymph node dissection. Thoracoscopic assistance is almost always used. Non-routine surgical procedures involve complex approaches such as broncho-/angio-plasty, combined resection with adjacent structures, and perioperative adjuvant treatment.
Since its establishment in 1992, our department has been one of the most active leaders in the field of lung cancer in Japan. Moreover, it has been an active participant in international and national scientific venues. This year, in addition to 16 scientific papers published in English, our department made 30 presentations: four international, 23 national, and four regional.
Our team and what we do
The Department of Thoracic Surgery is presently composed of four consultant surgeons including a chief and eight or nine residents.
Our department has adopted a team approach in patient treatment and resident training. Potential surgical intervention candidate cases are presented every Tuesday evening at a multidisciplinary team conference of thoracic surgeons, oncology physicians, radiologists, and residents. Each case is thoroughly and vigorously reviewed and discussed. To improve the English fluency of staff members and residents in preparation for international presentations, and to better involve visiting physicians from other countries, treatment modality discussions are conducted in English. Moreover, selected patients'records are radiologically and cytopathologically reviewed every Friday morning. These reviews aim to improve the interpretation of radiologic indications to pathology findings, accurately evaluate surgical indications, and upgrade knowledge on rare histologies. We believe that these activities improve the knowledge base, treatment indications, and surgical treatment.
For non-small cell histology, primary pulmonary carcinomas in clinical stages I/II and IIIA without bulky or multistation-involved mediastinal nodes, and primary pulmonary small cell carcinomas in clinical stage I, surgical resection is indicated for cure. Optimum treatment modalities are being sought via clinical trials with the aim of improving the poor prognosis of patients with bulky or clinically and histologically proven multistation mediastinal lymph node metastases, with disease invading the neighboring vital structures, or with small cell cancers in clinical stage II and later.
Resection of metastatic lung tumor is attempted based on modified Thomfold's criteria after consultation with the patient. The majority of these cases are metastases from colorectal carcinomas, while most of the mediastinal tumors are thymic epithelial tumors.
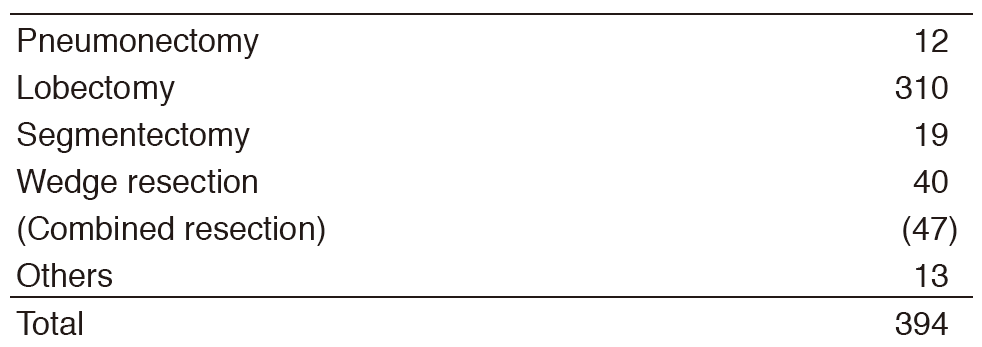
The surgical procedures of the Department of Thoracic Surgery have generally remained similar for the past decade, but we have employed port-access thoracoscopic surgery more often for the last several years. Approximately 20% of the surgeries are completed via a 3-port access, and 70% of the surgeries are video-thoracoscopically assisted. To date, an average postoperative hospital stay of patients in our department has been improved and become shorter, three days being the shortest with a median of seven days for cases of primary lung cancer. These shorter hospital stays are achieved with a slightly better complication rate than the normal rate. This year, 30-day operative mortality occurred in two patients undergoing surgery for primary lung cancer.
Research activities
Research in the area of combined treatment, especially immunotherapy, has now advanced to clinical trials. It is the goal for researchers in our department to acquire a basic understanding of the cellular and molecular mechanisms leading to the development and progression of lung cancer and apply these findings to further the development of immunotherapy-based prevention and treatment strategies.
Clinical trials
There are the following prospective trials in this department.
1.Primary investigator and a member of an organized trial of TS-1 vs. UFT adjuvant chemotherapy for completely resected pathologic stage I (> 2 cm) non-small cell lung cancer [JCOG 0707, phase III, patient accrual completed].
2.Primary investigator and a member of an organized trial of sublobar resection for peripheral GGO dominant cT1aN0M0 lung adenocarcinomas [JCOG 0804, phase II, patient accrual completed].
3.Study coordinator and a member of an organized trial of segmental resection vs. lobectomy for peripheral T1aN0M0 non-small cell lung cancers [JCOG 0802, phase III, patient accrual completed].
4.Study coordinator and a member of an organized trial of sublobar resection for peripheral GGO dominant cT1bN0M0 lung adenocarcinomas [JCOG 1211, phase III, patient accrual completed]
5.Primary investigator and a member of an organized trial of Cisplatin/Pemetrexed vs. Cisplatin/Vinorelbine adjuvant chemotherapy for completely resected pathologic stage II-IIIA non-small cell lung cancer [JIPANG, phase III, patient accrual ongoing].
6.A member of an organized trial of Human Atrial Natriuretic Peptide during perioperative period for completed resectable non-small cell lung cancer [JANP, randomized phase II, patient accrual ongoing].
7.A member of an organized trial of postoperative maintenance adjuvant immunotherapy with S-588410 for completed resected stage II-IIIA non-small cell lung cancer [S-588410, phase II, patient accrual ongoing]
Education
Our training program is to educate residents by expanding their knowledge and technical skills in the treatment of lung cancer, other thoracic malignancies, and benign tumors, such as hamartoma and mediastinal cystic lesions. In addition, we seek to instill in the trainee a desire for continued introspection and self-education, open communication between all health care providers, while maintaining a respectful and professional demeanor.
Future prospects
Treatment advances in thoracic cancers including lung, mesothelioma, thymic malignancies and lung metastases have been slow to develop, even though these cancers are among the most common clinical problems. This clinical and laboratory research is vital to making progress.
List of papers published in 2016
Journal
1.Shiraishi K, Okada Y, Takahashi A, Kamatani Y, Momozawa Y, Ashikawa K, Kunitoh H, Matsumoto S, Takano A, Shimizu K, Goto A, Tsuta K, Watanabe S, Ohe Y, Watanabe Y, Goto Y, Nokihara H, Furuta K, Yoshida A, Goto K, Hishida T, Tsuboi M, Tsuchihara K, Miyagi Y, Nakayama H, Yokose T, Tanaka K, Nagashima T, Ohtaki Y, Maeda D, Imai K, Minamiya Y, Sakamoto H, Saito A, Shimada Y, Sunami K, Saito M, Inazawa J, Nakamura Y, Yoshida T, Yokota J, Matsuda F, Matsuo K, Daigo Y, Kubo M, Kohno T. Association of variations in HLA class II and other loci with susceptibility to EGFR-mutated lung adenocarcinoma. Nat Commun, 7:12451, 2016
2.Hishida T, Nomura S, Yano M, Asamura H, Yamashita M, Ohde Y, Kondo K, Date H, Okumura M, Nagai K. Long-term outcome and prognostic factors of surgically treated thymic carcinoma: results of 306 cases from a Japanese Nationwide Database Study. Eur J Cardiothorac Surg, 49:835-841, 2016
3.Hishida T, Yoshida J, Aokage K, Nagai K, Tsuboi M. Postoperative oligo-recurrence of non-small-cell lung cancer: clinical features and survivaldagger. Eur J Cardiothorac Surg, 49:847-853, 2016
4.Watanabe K, Tsuboi M, Sakamaki K, Nishii T, Yamamoto T, Nagashima T, Ando K, Ishikawa Y, Woo T, Adachi H, Kumakiri Y, Maehara T, Nakayama H, Masuda M. Postoperative follow-up strategy based on recurrence dynamics for non-small-cell lung cancer. Eur J Cardiothorac Surg, 49:1624-1631, 2016
5.Zenke Y, Umemura S, Motegi A, Furukawa K, Kirita K, Matsumoto S, Yoh K, Niho S, Ohmatsu H, Tsuboi M, Akimoto T, Goto K. Acute and Progressive Tracheal Stenosis after Proton Beam Therapy with Concurrent Chemotherapy for Non-Small Cell Lung Cancer. J Thorac Oncol, 11:1181-1183, 2016
6.Mimae T, Suzuki K, Tsuboi M, Ikeda N, Takamochi K, Aokage K, Shimada Y, Miyata Y, Okada M. Severity of lung fibrosis affects early surgical outcomes of lung cancer among patients with combined pulmonary fibrosis and emphysema. Medicine (Baltimore), 95:e4314, 2016
7.Iwata T, Yoshino I, Yoshida S, Ikeda N, Tsuboi M, Asato Y, Katakami N, Sakamoto K, Yamashita Y, Okami J, Mitsudomi T, Yamashita M, Yokouchi H, Okubo K, Okada M, Takenoyama M, Chida M, Tomii K, Matsuura M, Azuma A, Iwasawa T, Kuwano K, Sakai S, Hiroshima K, Fukuoka J, Yoshimura K, Tada H, Nakagawa K, Nakanishi Y. A phase II trial evaluating the efficacy and safety of perioperative pirfenidone for prevention of acute exacerbation of idiopathic pulmonary fibrosis in lung cancer patients undergoing pulmonary resection: West Japan Oncology Group 6711 L (PEOPLE Study). Respir Res, 17:90, 2016
8.Hishida T, Yoshida J, Aokage K, Nagai K, Tsuboi M. Long-term outcome of surgical resection for residual or regrown advanced non-small cell lung carcinomas following EGFR-TKI treatment: report of four cases. Gen Thorac Cardiovasc Surg, 64:429-433, 2016
9.Hishida T, Miyaoka E, Yokoi K, Tsuboi M, Asamura H, Kiura K, Takahashi K, Dosaka-Akita H, Kobayashi H, Date H, Tada H, Okumura M, Yoshino I. Lobe-Specific Nodal Dissection for Clinical Stage I and II NSCLC: Japanese Multi-Institutional Retrospective Study Using a Propensity Score Analysis. J Thorac Oncol, 11:1529-1537, 2016
10.Shimada Y, Suzuki K, Okada M, Nakayama H, Ito H, Mitsudomi T, Saji H, Takamochi K, Kudo Y, Hattori A, Mimae T, Aokage K, Nishii T, Tsuboi M, Ikeda N. Feasibility and efficacy of salvage lung resection after definitive chemoradiation therapy for Stage III non-small-cell lung cancer. Interact Cardiovasc Thorac Surg, 23:895-901, 2016
11.Aramaki N, Ishii G, Yamada E, Morise M, Aokage K, Kojima M, Hishida T, Yoshida J, Ikeda N, Tsuboi M, Ochiai A. Drastic morphological and molecular differences between lymph node micrometastatic tumors and macrometastatic tumors of lung adenocarcinoma. J Cancer Res Clin Oncol, 142:37-46, 2016
12.Neri S, Hashimoto H, Kii H, Watanabe H, Masutomi K, Kuwata T, Date H, Tsuboi M, Goto K, Ochiai A, Ishii G. Cancer cell invasion driven by extracellular matrix remodeling is dependent on the properties of cancer-associated fibroblasts. J Cancer Res Clin Oncol, 142:437-446, 2016
13.Hisakane K, Saruwatari K, Fujii S, Kirita K, Umemura S, Matsumoto S, Yoh K, Niho S, Ohmatsu H, Kuwata T, Ochiai A, Gemma A, Tsuboi M, Goto K, Ishii G. Unique intravascular tumor microenvironment predicting recurrence of lung squamous cell carcinoma. J Cancer Res Clin Oncol, 142:593-600, 2016
14.Sekihara K, Hishida T, Ikemura S, Saruwatari K, Morise M, Kuwata T, Fujii S, Kojima M, Ochiai A, Funai K, Aokage K, Yoshida J, Tsuboi M, Ishii G. The association of intravascular stromal cells with prognosis in high-grade neuroendocrine carcinoma of the lung. J Cancer Res Clin Oncol, 142:905-912, 2016
15.Saruwatari K, Ikemura S, Sekihara K, Kuwata T, Fujii S, Umemura S, Kirita K, Matsumoto S, Yoh K, Niho S, Ohmatsu H, Ochiai A, Kohrogi H, Tsuboi M, Goto K, Ishii G. Aggressive tumor microenvironment of solid predominant lung adenocarcinoma subtype harboring with epidermal growth factor receptor mutations. Lung Cancer, 91:7-14, 2016
16.Matsuzawa R, Kirita K, Kuwata T, Umemura S, Matsumoto S, Fujii S, Yoh K, Kojima M, Niho S, Ohmatsu H, Ochiai A, Tsuboi M, Goto K, Ishii G. Factors influencing the concordance of histological subtype diagnosis from biopsy and resected specimens of lung adenocarcinoma. Lung Cancer, 94:1-6, 2016
17.Hata K, Yoshida J, Udagawa H, Hashimoto H, Fujii S, Hishida T, Kuwata T, Aokage K, Kojima M, Ochiai A, Suzuki K, Tsuboi M, Ishii G. The difference in Ezrin-pAkt signaling axis between lepidic and papillary predominant invasive adenocarcinomas of the lung. J Cancer Res Clin Oncol, 142:1421-1430, 2016
18.Suzuki S, Aokage K, Hishida T, Yoshida J, Kuwata T, Yamauchi C, Tsuboi M, Ishii G. Interstitial growth as an aggressive growth pattern in primary lung cancer. J Cancer Res Clin Oncol, 142:1591-1598, 2016
19.Suda Y, Neri S, Hashimoto H, Higuchi Y, Ishibashi M, Sugano M, Masutomi K, Tsuboi M, Ochiai A, Ishii G. Clonal heterogeneity in osteogenic potential of lung cancer-associated fibroblasts: promotional effect of osteogenic progenitor cells on cancer cell migration. J Cancer Res Clin Oncol, 142:1487-1498, 2016
20.Naito M, Aokage K, Saruwatari K, Hisakane K, Miyoshi T, Hishida T, Yoshida J, Masato S, Kojima M, Kuwata T, Fujii S, Ochiai A, Sato Y, Tsuboi M, Ishii G. Microenvironmental changes in the progression from adenocarcinoma in situ to minimally invasive adenocarcinoma and invasive lepidic predominant adenocarcinoma of the lung. Lung Cancer, 100:53-62, 2016