HOME > Publication & Reports > Annual Report 2016 > Hospital
Department of Colorectal Surgery
Yukihide Kanemitsu, Dai Shida, Shunsuke Tsukamoto, Hiroki Ochiai, Masahiro Tanaka, Gouki Morizono
Introduction
The Department of Colorectal Surgery deals with colorectal cancer and allied malignancies in the colon and rectum. Liver metastasis from colorectal cancer is treated in cooperation with the Department of Hepatobiliary and Pancreatic Surgery. Lung metastasis from colorectal cancer is also treated in cooperation with the Department of Thoracic Surgery. Although surgery is still the main treatment modality for colorectal cancer, multidisciplinary treatments including radiotherapy and chemotherapy are important in advanced cancer. We have multidisciplinary meetings with the Department of Gastrointestinal Medical Oncology, the Department of Endoscopy, the Department of Diagnostic Radiology, and the Department of Pathology and Clinical Laboratories every week, and decide treatment strategy by a multidisciplinary team (MDT) before treatment is performed.
Our team and what we do
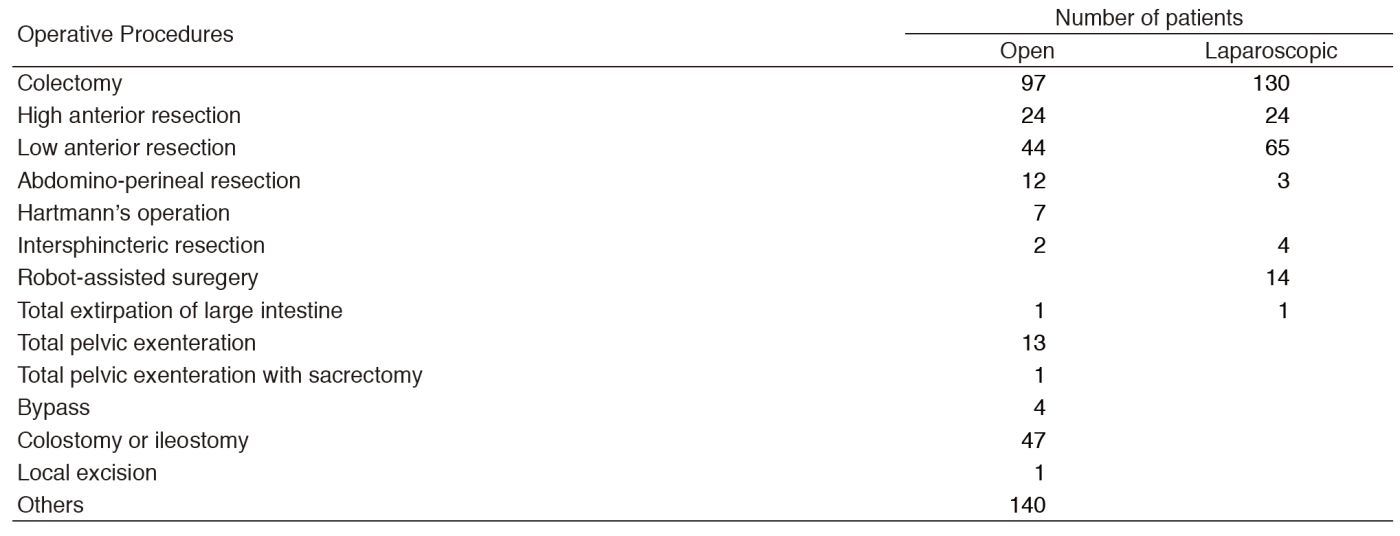
In the Department of Colorectal Surgery, four surgeons perform more than 600 colorectal operations per year, which is top-class in Japan, and we always aim to improve survival rate with safe surgery associated with less complications. The length of hospital stay is as short as seven days after surgery in laparotomy, laparoscopic surgery, and robot-assisted surgery, which allows more patients to receive surgical treatment with fewer beds.
There are four staff surgeons, one chief resident, and three or four rotating residents. Every morning (7:30-8:30), we have a morning conference and rounds in wards 15A and B. MDT meeting is held for cancer patients as a form of institutionalized communication every Tuesday morning (7:15-8:00), and a conference is held for the diagnosis of colorectal cancer: colorectal surgeons, endoscopists, and radiologists discuss the diagnosis for preoperative patients every Tuesday evening (18:30-19:30). Every Wednesday morning (7:00-7:30), a conference is held for the treatment of colorectal cancer: colorectal surgeons discuss treatments for preoperative and postoperative patients. Ten to twelve operations are performed a week in our department.
* Robot-assisted surgery:
In our department, we have been performing robot-assisted rectal surgeries, in which robotic surgery technology is applied to rectal cancer treatment, since March 2014. It is considered that rectal cancer surgery using the Da Vinci surgical system enables more intricate and precise operations because the doctor performs surgery with robotic support. It also enables safer and less invasive surgery since accurate image data can be obtained from three dimensions. The field of robot-assisted surgery is expected to play an important role in next-generation surgery. We have already confirmed the safety and feasibility of this new robot-assisted rectal surgery in the clinical study in 30 patients. Currently, the surgery is performed as a treatment option that is not covered by the insurance.
Research activities
Patients with advanced rectal cancers are treated with conventional surgery. Adjuvant chemotherapy is being used in stage III colorectal cancer patients in a clinical setting. Although preoperative radiotherapy is not performed routinely for advanced rectal cancer, patients with T4b rectal cancers or rectal cancers with multiple lymph node metastases are treated with preoperative chemoradiotherapy and surgery. Patients with symptoms caused by unresectable tumors are treated with palliative surgery including palliative resection, bypass, and stoma before chemotherapy. To evaluate the survival benefit and safety of primary resection plus chemotherapy compared to chemotherapy alone in asymptomatic stage IV colorectal cancer with synchronous unresectable metastatic disease, a randomized controlled trial comparing resection of primary tumor plus chemotherapy with chemotherapy alone in incurable stage IV colorectal cancer is ongoing (The Japan Clinical Oncology Group (JCOG) 1007, iPACS). Another randomized controlled trial is ongoing to evaluate the non-inferiority of overall survival of laparoscopic surgery to open surgery for palliative resection of primary tumor in incurable stage IV colorectal cancer (JCOG 1107, ENCORE). Symptomatic, stage IV colorectal cancer patients with non-curable metastasis are pre-operatively randomized to either open or laparoscopic colorectal resection. Patients with resectable liver metastasis are treated in cooperation with the Department of Hepatobiliary and Pancreatic Surgery and adjuvant chemotherapy regimens are being evaluated in a clinical trial (JCOG 0603 study). To confirm the superiority of perioperative chemotherapy, a randomized phase II/III trial was started in May 2015 comparing perioperative versus postoperative chemotherapy with modified infusional fluorouracil and folinic acid with oxaliplatin (mFOLFOX6) for lower rectal cancer patients with suspected lateral pelvic node metastasis (JCOG 1310).
We also carry out basic research in cooperation with scientists at the National Cancer Center Research Institute and the identification of a suitable treatment based on such a prediction is one of our important goals.
Clinical trials
Our department plays a central role in conducting multi-institutional clinical trials in Japan. Y. Shimada is a representative of the Colorectal Cancer Group of the JCOG. Our department is participating in nine phase III JCOG studies.
1)JCOG 0212: A randomized study that compares mesorectal excision (ME) to ME with pelvic lateral lymph node dissection for clinical stage II or stage III lower rectal cancer patients. A total of 701 eligible patients were enrolled and recruitment is complete. Follow-up is ongoing.
2)JCOG 0603: A randomized study that compares adjuvant modified FOLFOX (5-FU + l-LV +Oxaliplatin) to surgery alone after hepatic resection for liver metastasis from colorectal cancer. A total of 170 patients have been enrolled and recruitment continues.
3)JCOG 1006: A randomized study that compares conventional techniques to the no-touch isolation technique for clinical T3 or T4 colon cancer. A total of 570 patients have been enrolled and recruitment continues.
4)JCOG 1007: A randomized controlled trial comparing resection of primary tumor plus chemotherapy with chemotherapy alone in incurable stage IV colorectal cancer is ongoing.
5)JCOG 1018: Randomized phase III study of mFOLFOX7 or CAPOX plus bevacizumab versus 5-Fluorouracil/leucovorin or capecitabine plus bevacizumab as first-line treatment in elderly patients with metastatic colorectal cancer is ongoing.
6)JCOG 1107: A randomized controlled trial comparing laparoscopic surgery with open surgery in palliative resection of primary tumors in incurable stage IV colorectal cancer is ongoing.
7)JCOG 1310: A phase II/III randomized controlled trial comparing perioperative versus postoperative chemotherapy with mFOLFOX6 for lower rectal cancer with suspected lateral pelvic node metastasis is ongoing.
8)JCOG 1410A: Japanese Observational Study to Evaluate the Accuracy of Preoperative Imaging Diagnosis for Lateral Pelvic Lymph Node Metastasis in Rectal Cancer is ongoing.
9)JCOG 1506A: Prognostic or predictive biomarker study in patients who underwent surgery with/without postoperative chemotherapy for stage II/III colorectal cancer is ongoing.
Future prospects
* Development of a new laparoscopic surgical system using 8K Super Hi-Vision technology:
At the National Cancer Center Hospital, a national research project working on the development of a new laparoscopic surgical system and the utilization of high definition image data using 8K Super Hi-Vision technology has been initiated. With this project, further improvement of the treatment outcome of patients with colorectal cancer is expected in the future.
List of papers published in 2016
Journal
1.Matsumoto M, Nakajima T, Kakugawa Y, Sakamoto T, Kuribayashi S, Otake Y, Matsuda T, Kanemitsu Y, Taniguchi H, Saito Y. Surveillance using capsule endoscopy is safe in post-colectomy patients with familial adenomatous polyposis: a prospective Japanese study. Fam Cancer, 15:75-83, 2016
2.Saito S, Fujita S, Mizusawa J, Kanemitsu Y, Saito N, Kinugasa Y, Akazai Y, Ota M, Ohue M, Komori K, Shiozawa M, Yamaguchi T, Akasu T, Moriya Y. Male sexual dysfunction after rectal cancer surgery: Results of a randomized trial comparing mesorectal excision with and without lateral lymph node dissection for patients with lower rectal cancer: Japan Clinical Oncology Group Study JCOG0212. Eur J Surg Oncol, 42:1851-1858, 2016
3.Ishihara S, Kanemitsu Y, Murono K, Otani K, Yasuda K, Nishikawa T, Tanaka T, Tanaka J, Kiyomatsu T, Kawai K, Hata K, Nozawa H, Kazama S, Yamaguchi H, Sunami E, Sugihara K, Watanabe T, . Oncological benefit of lateral pelvic lymph node dissection for rectal cancer treated without preoperative chemoradiotherapy: a multicenter retrospective study using propensity score analysis. Int J Colorectal Dis, 31:1315-1321, 2016
4.Konishi T, Ishida H, Ueno H, Kobayashi H, Hinoi T, Inoue Y, Ishida F, Kanemitsu Y, Yamaguchi T, Tomita N, Matsubara N, Watanabe T, Sugihara K, . Feasibility of laparoscopic total proctocolectomy with ileal pouch-anal anastomosis and total colectomy with ileorectal anastomosis for familial adenomatous polyposis: results of a nationwide multicenter study. Int J Clin Oncol, 21:953-961, 2016
5.Saito Y, Hinoi T, Ueno H, Kobayashi H, Konishi T, Ishida F, Yamaguchi T, Inoue Y, Kanemitsu Y, Tomita N, Matsubara N, Komori K, Kotake K, Nagasaka T, Hasegawa H, Koyama M, Ohdan H, Watanabe T, Sugihara K, Ishida H, . Risk Factors for the Development of Desmoid Tumor After Colectomy in Patients with Familial Adenomatous Polyposis: Multicenter Retrospective Cohort Study in Japan. Ann Surg Oncol, 23:559-565, 2016
6.Inoue Y, Ishida H, Ueno H, Kobayashi H, Yamaguchi T, Konishi T, Tomita N, Matsubara N, Ishida F, Hinoi T, Kanemitsu Y, Watanabe T, Sugihara K, . Therapeutic approaches for patients with coexisting familial adenomatous polyposis and colorectal cancer. Jpn J Clin Oncol, 46:819-824, 2016
7.Shida D, Hamaguchi T, Ochiai H, Tsukamoto S, Takashima A, Boku N, Kanemitsu Y. Prognostic Impact of Palliative Primary Tumor Resection for Unresectable Stage 4 Colorectal Cancer: Using a Propensity Score Analysis. Ann Surg Oncol, 23:3602-3608, 2016
8.Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, Tsubosa Y, Satoh T, Yokomizo A, Fukuda H, Sasako M, . Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today, 46:668-685, 2016
9.Inoki K, Nakajima T, Sekine S, Sugano K, Tsukamoto S, Yamada M, Mutoh M, Sakamoto T, Matsuda T, Sekiguchi M, Ushiama M, Yoshida T, Sakamoto H, Kanemitsu Y, Saito Y. Depressed-type submucosal invasive colorectal cancer in a patient with Lynch syndrome diagnosed using short-interval colonoscopy. Dig Endosc, 28:749-754, 2016