HOME > Publication & Reports > Annual Report 2016 > Hospital
Department of Hepatobiliary and Pancreatic Surgery
Kazuaki Shimada, Minoru Esaki, Yoji Kishi, Satoshi Nara, Toshimitsu Iwasaki
Introduction
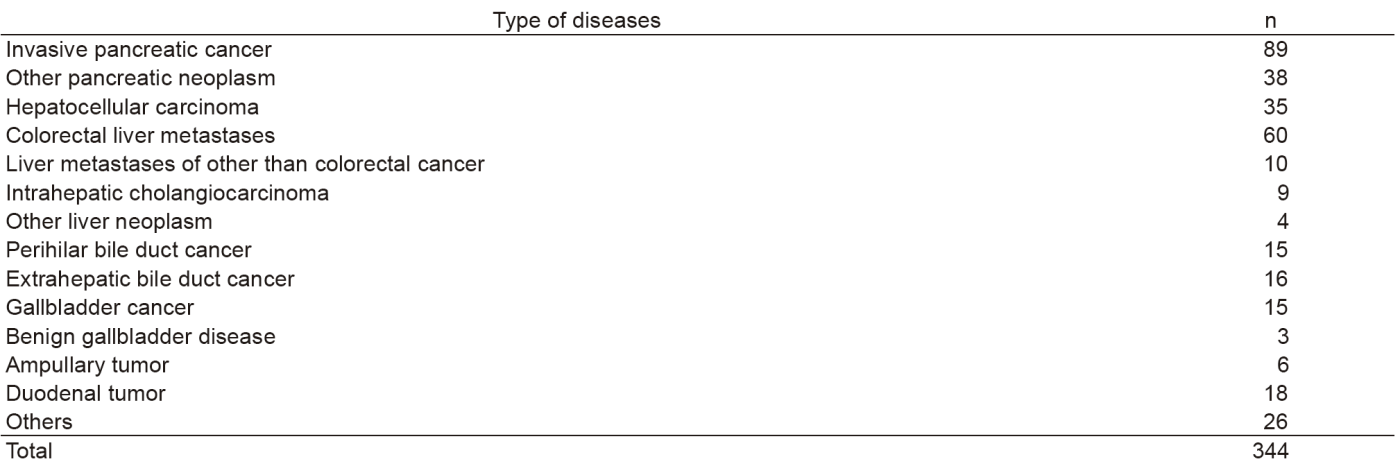
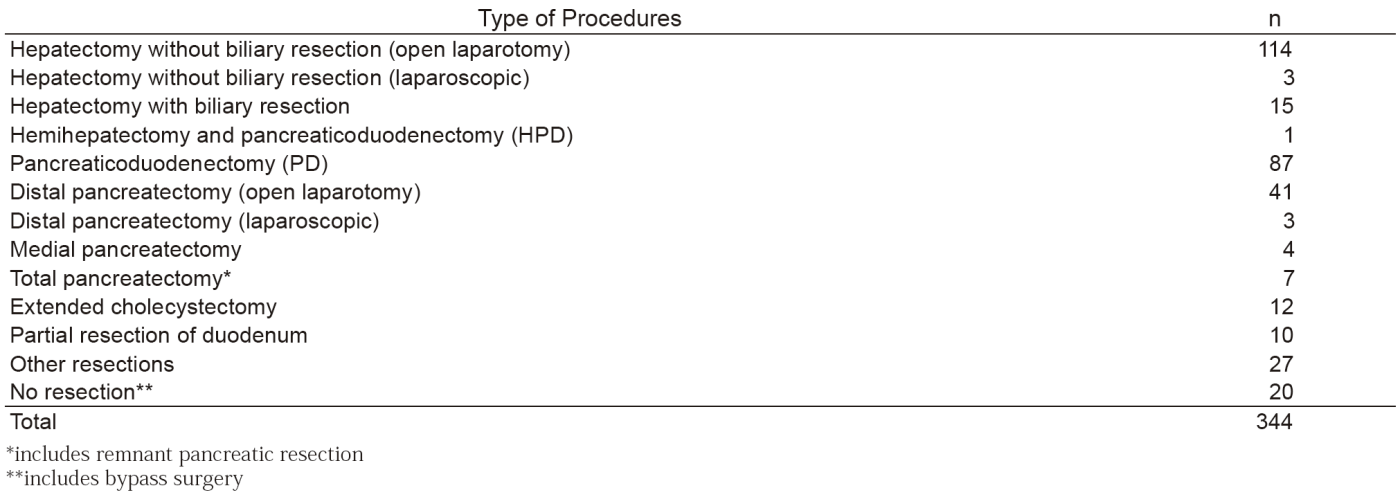
The Department of Hepatobiliary and Pancreatic (HBP) Surgery deals with malignant neoplasms arising from the liver, biliary tract including the gallbladder, and pancreas. We conduct aggressive surgical treatment and multidisciplinary treatment in cooperation with the Department of Diagnostic Radiology, the Department of Hepatobiliary and Pancreatic (HBP) Oncology, and the Pathology Division.
Our team and what we do
Our department consists of four staff surgeons and we perform more than 300 surgeries each year, along with one chief resident, and three or four residents. Occasionally, trainees from Japan and abroad join our group.
1. Operation and perioperative care
One staff surgeon and one resident are in charge of each patient, that conduct the operation and provide postoperative care. The chief resident attends almost all operations, supervises the residents, and manages the care of all inpatients.
2. Conferences
We hold several clinical and educational conferences on the treatment of HBP malignancies. At the "Ward Conference", the clinical conditions of the perioperative patients and surgical strategies for preoperative cases are discussed. At the "Cherry Conference", surgeons and radiologists discuss imaging studies of patients scheduled for surgery. The "HBP Case Conference" is held by surgeons and medical oncologists to discuss treatment strategies. The "Micro Conference" is a pathological conference on postoperative cases, where surgeons, radiologists, and pathologists participate in the discussion.
3. Surgical strategies for HBP malignancies
Hepatocellular carcinoma (HCC): Surgical resection is usually indicated in patients with solitary or only a few tumors, and with favorable hepatic function. A huge tumor or HCC with macroscopic vasculobiliary tumor thrombosis are also indicated for resection as long as sufficient hepatic function and remnant liver volume is expected. Alternative treatments other than hepatectomy are performed in cooperation with medical oncologists and radiologists.
Pancreatic cancer: Multidisciplinary treatments with curative resection followed by adjuvant chemotherapy is the standard strategy. When the pancreatectomy is indicated for locally advanced cancer initially treated with systemic chemotherapy, there is still a controversial issue.
Biliary cancer - cholangiocarcinoma and gall bladder cancer: Based on careful imaging evaluations of cancer extension, a wide variety of surgical resections can be applied to biliary cancer. Major resection including pancreatoduodenectomy and/or extended hemihepatectomy with extrahepatic bile duct resection with or without vascular reconstruction is frequently indicated. Safe and curative resection with careful perioperative management is mandatory.
Laparoscopic surgery: For liver tumors located in the peripheral site, laparoscopic lateral bisegmentectomy or partial resection is considered as a choice of treatment. Laparoscopic distal pancreatectomy is considered for slowly growing malignant tumors.
Research activities
Dr. Shimada et al. conducts two multiinstitutional randomized trials. One is to evaluate the safety of drain tube free hepatectomy (ND-trial), and the other is to evaluate the efficacy of administrating digestive enzymes to prevent postoperative hepatic steatosis in patients who underwent pancreaticoduodenectomy (ESOP Trial). Dr. Kishi attends an international collaboration project by EORTC (European Organisation for Research and Treatment of Cancer) and the JCOG (Japan Clinical Oncology Group) as a Japanese side manager. The project is to evaluate the accuracy of Diffusion-weighted Magnetic Resonance Imaging for the assessment of diminishing colorectal liver metastases by chemotherapy (DREAM study).
Each staff attends three to four domestic and international academic meetings per year. Residents and chief residents also have opportunities to make a presentation with the assistance of staff surgeons.
Clinical trials
In addition to the above mentioned RCTs (ND-trial and ESOP trial) and DREAM study, we attend a JCOG1202 phase III trial that evaluates the efficacy of adjuvant S-1 treatment in patients who underwent curative surgical resection for biliary tract cancer (ASCOT trial).
Education
Each resident attends one to two major HBP surgeries mainly as the first assistant. They also have the chance to be an operator depending on their skill. For each case, they learn how to decide the indication and type of procedure based on preoperative images. In the operation room, the residents learn not only each step of HBP surgery, but also tips on how to help safely proceed with the surgery. The chief resident trains them in a two-year program. In the first year, they devote themselves to the management of all inpatients and attend basically every surgery. Depending on the development of their skills, they have the opportunity to be an operating surgeon for major HBP surgery. In the second year, the chief resident works on research studies and publishes several English papers. Motivated residents also have the opportunity to make presentations in academic meetings and write English papers.
Visitors from both domestic and foreign institutions are welcome anytime.
Future prospects
HBP malignancy often requires technically demanding surgical procedures, whereas the long-term prognosis so far is not satisfactory. Our most important mission is to establish more safe and feasible surgical techniques including perioperative patient management, and to promote survival outcomes by multidisciplinary approaches. Due to the recent advances of chemotherapy, we have experienced a few patients who achieved curative surgical resection for initially unresectable pancreatic cancer due to local advancement. So the feasibility of conversion therapy should be assessed prospectively. We continue making efforts to create new skills and treatment strategies. In addition, clinical trials to explore unclarified clinical questions are expected.
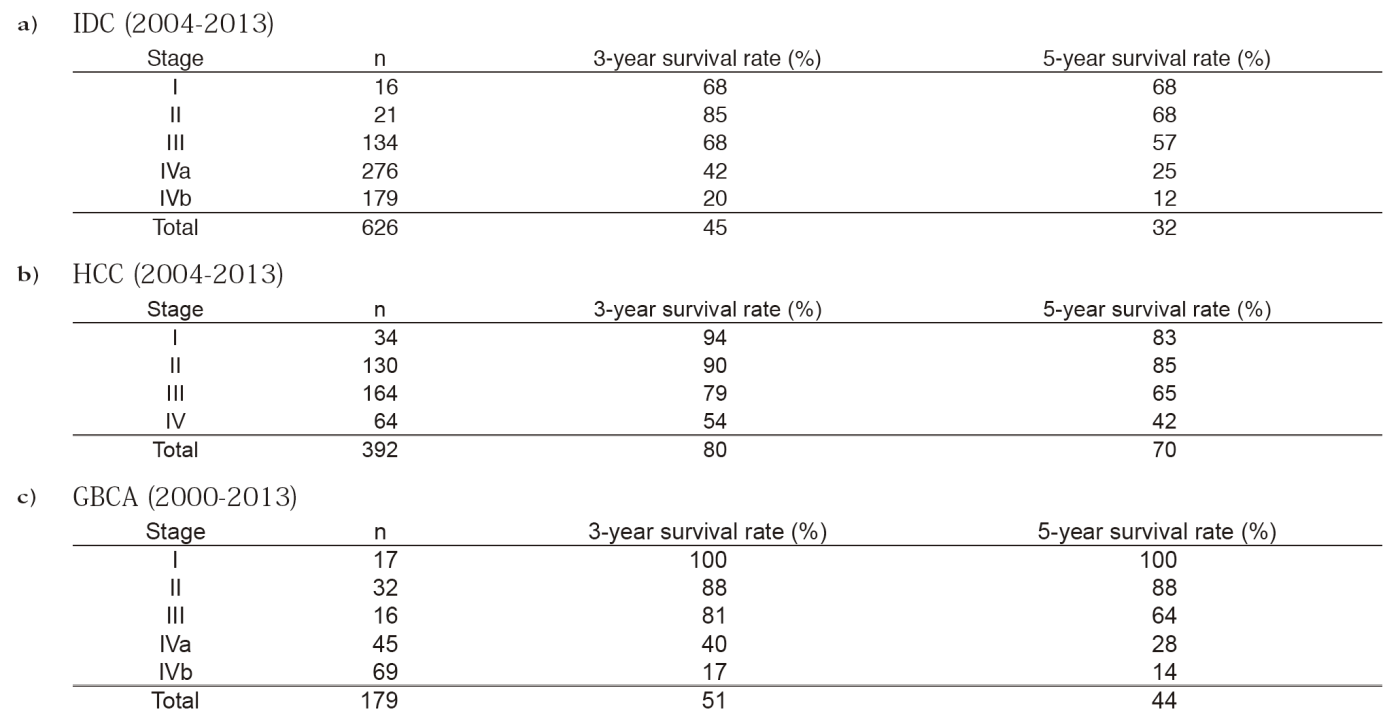
Table 3. Postoperative survival rates of the patients with a) pancreatic invasive ductal cancer (IDC),b) hepatocellular carcinoma (HCC), and c) gallbladder cancer (GBCA)
List of papers published in 2016
Journal
1.Akizuki N, Shimizu K, Asai M, Nakano T, Okusaka T, Shimada K, Inoguchi H, Inagaki M, Fujimori M, Akechi T, Uchitomi Y. Prevalence and predictive factors of depression and anxiety in patients with pancreatic cancer: a longitudinal study. Jpn J Clin Oncol, 46:71-77, 2016
2.Midorikawa Y, Takayama T, Higaki T, Nakayama H, Yamamoto M, Ariizumi S, Shimada K, Kokudo N, Tsuji S, Tsuchiya K, Kurosaki M, Izumi N. Early hepatocellular carcinoma as a signaling lesion for subsequent malignancy. Jpn J Clin Oncol, 46:1102-1107, 2016
3.Midorikawa Y, Takayama T, Nara S, Hashimoto T, Omichi K, Ebisawa K, Higaki T, Tsuji S, Sakamoto H, Shimada K, Makuuchi M. No Need of Immediate Treatment for Hypovascular Tumors Associated with Hepatocellular Carcinoma. World J Surg, 40:2460-2465, 2016
4.Hori S, Shimada K, Ino Y, Oguro S, Esaki M, Nara S, Kishi Y, Kosuge T, Hattori Y, Sukeda A, Kitagawa Y, Kanai Y, Hiraoka N. Macroscopic features predict outcome in patients with pancreatic ductal adenocarcinoma. Virchows Arch, 469:621-634, 2016
5.Tanaka M, Kishi Y, Esaki M, Nara S, Miyake M, Hiraoka N, Nagino M, Shimada K. Feasibility of Routine Application of Gadoxetic Acid-Enhanced MRI in Combination with Diffusion-Weighted MRI for the Preoperative Evaluation of Colorectal Liver Metastases. Ann Surg Oncol, 23:3991-3998, 2016
6.Hori M, Onaya H, Hiraoka N, Yamaji T, Kobayashi H, Takahashi M, Mutoh M, Shimada K, Nakagama H. Evaluation of the degree of pancreatic fatty infiltration by area-based assessment of CT images: comparison with histopathology-based and CT attenuation index-based assessments. Jpn J Radiol, 34:667-676, 2016
7.Kishi Y, Shimada K, Nara S, Esaki M, Kosuge T. The type of preoperative biliary drainage predicts short-term outcome after major hepatectomy. Langenbecks Arch Surg, 401:503-511, 2016
8.Yoshida H, Shimada K, Kosuge T, Hiraoka N. A significant subgroup of resectable gallbladder cancer patients has an HER2 positive status. Virchows Arch, 468:431-439, 2016
9.Monma SE, Shimada K, Kishi Y, Nara S, Esaki M, Fujiki M, Miyamoto S, Hiraoka N. An extremely rare clinical manifestation of gallbladder cancer presenting with abdominal wall invasion with an erythematous skin break. Pathol Int, 66:302-304, 2016