HOME > Publication & Reports > Annual Report 2016 > Hospital
Department of Palliative Medicine
Eriko Satomi, Kaoru Nishijima, Daisuke Kiuchi, Koutarou Nomura
Introduction
The palliative care service started with a palliative care team of multidiciplenary professionals (palliative care specialists, psycho-oncologists, certified nurses, pharmacists, psychologists, Hospital Play Staff, acupuncturist) in the National Cancer Center Hospital (NCCH) in 1999 and the Department of Palliative Care and Psychooncology was established in 2010 with the reorganization of the NCCH. In 2013, the Department of Palliative Medicine started.
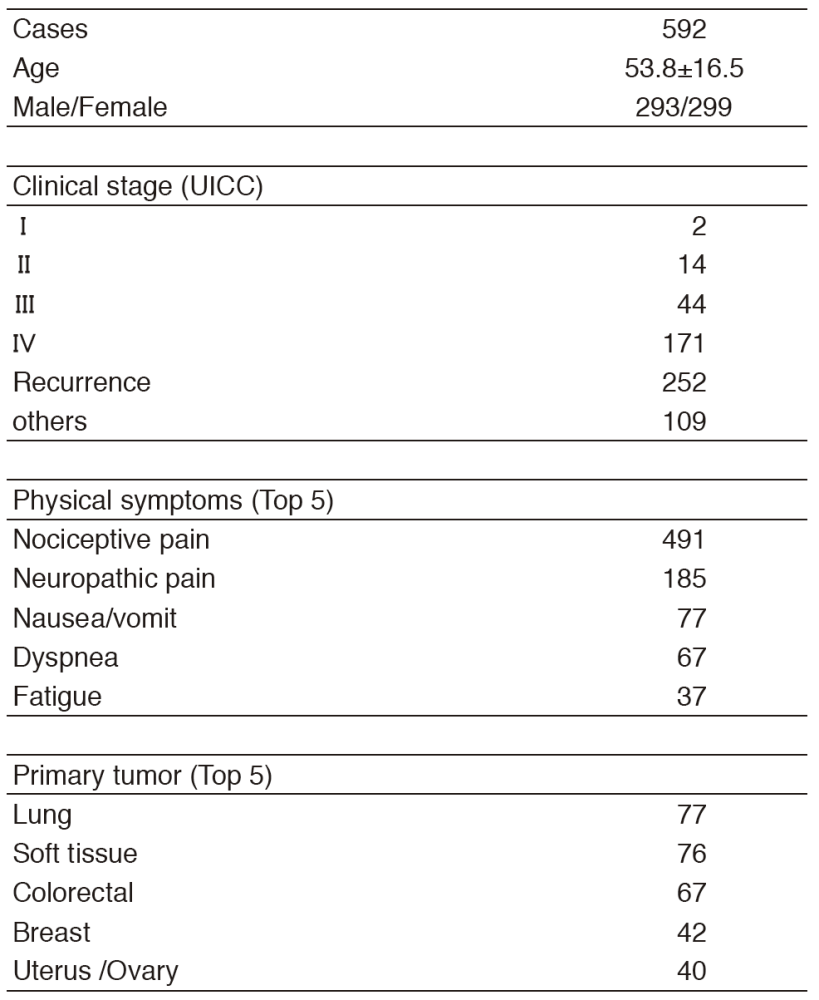
Table 1. Patient demography (2016)
Our team and what we do
We provide palliative care to patients and their families as members of the palliative care team collaborating with primary doctors, nurses, and other professionals to create an individualized palliative care plan. Our goals are:
- Relieve pain and other physical symptoms
- Focus on patients'emotional and spiritual concerns, and those of their caregiver
- Coordinate patients'care
- Improve the quality of life of patients with cancer
- Advance care planning
Research activities
We are participating and conducting multicenter observational studies and interventional studies for supportive and palliative care, and continuously planning palliative care researches for the innovation of palliative care.
Clinical trials
JORTC-PAL08 (Efficacy of duloxetine for cancer patients with neuropathic pain: Double blind, Randomized, Placebo controlled, exploratory trial), PHASE-R (Olanzapine for nausea and vomit :observational study), J-SUPPORT 1603 (Nurse-led, screening-triggered early specialized palliative care intervention program for advanced lung cancer patients randomized controlled trial) , EASED (East-Asian collaborative Study to Elucidate the Dying process) , etc.
Education
We have two training courses for doctors who will be palliative care specialists and for residents to learn primary palliative care. All the surgical and medical oncology residents in the NCCH need the knowledge and skills about primary supportive and palliative care in oncology. They participate in our team for four weeks and undergo on-the-job training for palliative medicine. It includes an opportunity to attend home hospice rounds in cooperation with the Chuo-ku Medical Association. A total of 22 residents finished the four-week palliative medicine course in 2016. One short-term resident and one chief resident registered for the specialized palliative care education course. They learned specialist palliative care in oncology including physical, psychosocial, and spiritual supportive care during anti-cancer therapy as well as end-of-life care, and support for patients'decision making and advance care planning.
List of papers published in 2016
Journal
1.Iwase S, Ishiki H, Watanabe A, Shimada N, Chiba T, Kinkawa J, Tojo A. Mapisal Versus Urea Cream as Prophylaxis for Capecitabine-Associated Hand-Foot Syndrome. J Clin Oncol, 34:391, 2016
2.Iwase S, Kawaguchi T, Yotsumoto D, Doi T, Miyara K, Odagiri H, Kitamura K, Ariyoshi K, Miyaji T, Ishiki H, Inoue K, Tsutsumi C, Sagara Y, Yamaguchi T. Efficacy and safety of an amino acid jelly containing coenzyme Q10 and L-carnitine in controlling fatigue in breast cancer patients receiving chemotherapy: a multi-institutional, randomized, exploratory trial (JORTC-CAM01). Support Care Cancer, 24:637-646, 2016
3.Takimoto K, Nishijima K, Ono M. Serratus Plane Block for Persistent Pain after Partial Mastectomy and Axillary Node Dissection. Pain Physician, 19:E481-486, 2016
Future prospects
We will continue to provide qualified palliative cancer care with an integrated palliative care model in clinical practice throughout the continuum of a person's disease, regardless of whether it is early or later in the course of the disease. And we will enhance our palliative care education program for specialists and oncologists. We also continuously conduct good palliative care researches in order to strengthen its evidence to improve palliative care practice.