Annual Report 2017
Department of Head and Neck Surgery
Ryuichi Hayashi, Takeshi Shinozaki, Toshifumi Tomioka, Wataru Okano, Masakazu Ikeda, Takahiko Nagaki, Yohei Morishita
Introduction
Surgical treatment of head and neck cancer must meet two contradictory requirements: (1) the resection volume must be sufficiently large to remove all cancer cells and (2) the resection volume should be sufficiently small to preserve important functions such as swallowing, speech, vision, and cosmetic appearance. The Department of Head and Neck Surgery resolves these conflicting requirements mainly by two distinct approaches: (1) conservative surgery and (2) extensive resection with microsurgical reconstruction. We have been developing various larynx-preserving operations since the establishment of the National Cancer Center (NCC). These procedures include a partial laryngectomy which is indicated for T1/T2 recurrent glottis carcinoma after radiotherapy. Another example of conservative surgery is partial laryngo-pharyngectomy with preservation of swallowing and voicing function for hypopharyngeal carcinoma. Recently, trans-oral resection for pharyngo-laryngeal cancer has been increasing as minimal invasive surgery. On the other hand, extensive resection with microsurgical reconstruction is designed to minimize loss of function following ablative surgery by employing the microsurgical transfer of various flaps.
Our team and what we do
The current treatment policy for head and neck cancer is multimodal therapy. To effectively implement available therapeutic modalities, four staff surgeons at our department work closely with plastic surgeons, radiotherapists, medical oncologists, pathologists, dentists, psycho-
oncologists, and nurses. To facilitate regular communication among the members of this large team, several weekly conferences are conducted.
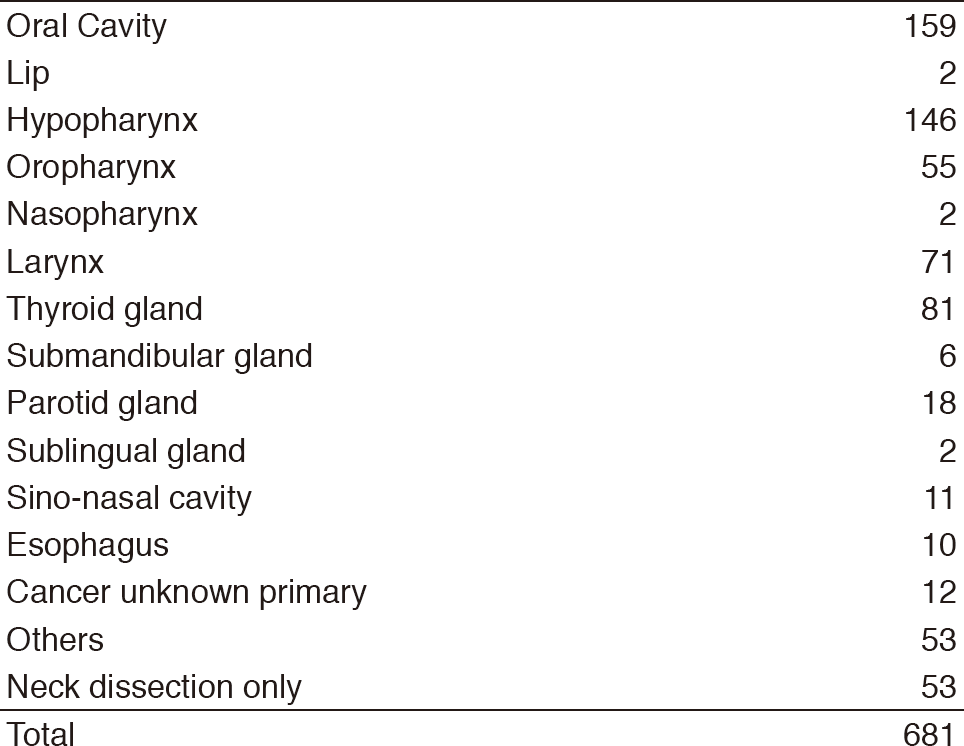
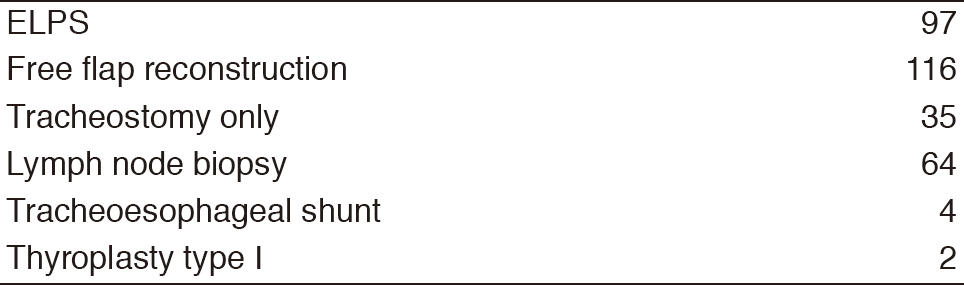
The number of operations was 681 cases (572 cases under general anesthesia, 109 cases under local anesthesia). Ninety-seven cases of all underwent endoscopic laryngo-pharyngeal surgery (ELPS) and 116 cases underwent free flap reconstruction (Tables 1, 2).
Research activities
1. Concomitant expression of ezrin and HER2 predicts distant metastasis and poor prognosis of patients with salivary gland carcinomas
Salivary gland carcinomas (SGCs) exhibit heterogeneous biological behaviors, including the formation of distant metastases, which is a critical event associated with poor prognosis. Ezrin, which is a member of the ezrin-radixin-
moesin family of plasma membrane-cytoskeleton linker proteins, may provide a marker for metastasis and poor survival of patients with cancer. The aim of the present study was to investigate the relationship between ezrin expression and the expression of HER2, p53, and Ki-67 as well as clinicopathological factors in SGCs. Multivariate analysis demonstrated that high ezrin expression was an independent prognostic factor for shorter overall survival (hazard ratio, 2.11 [1.09-4.05]; P=.027). Furthermore, concomitant high expression of ezrin and HER2 overexpression correlated significantly with shorter disease-free survival and overall survival as well as a high incidence of distant metastasis (P<.001). These findings indicate that ezrin and HER2 expression in patients with SGCs represents a high-grade histopathological subtype that requires adjuvant therapy, including molecularly targeted therapies, to decrease the risk of subsequent metastasis.
Clinical trials
We participate in "Phase II/III Trial of Postoperative Chemoradiotherapy Comparing 3-Weekly Cisplatin with Weekly Cisplatin in High-risk Patients with Squamous Cell Carcinoma of Head and Neck (JCOG1008)", "Dose finding and confirmatory trial of superselective intra-
arterial infusion of cisplatin and concomitant radiotherapy for patients with locally advanced maxillary sinus cancer (JCOG 1212)", and "Randomized phase III study to evaluate the value of omission of prophylactic neck dissection for stage I/II tongue cancer: Japan Clinical Oncology Group study (JCOG1601)". TOS-J trial (Phase II/III study of transoral surgery for superficial head and neck cancer in Japan) has been conducted in order to evaluate the safety and effectiveness of transoral surgery for superficial head and neck cancer.
Education
Two residents were recruited to our department in 2017. Six medical students visited our department for training. Our department was assigned as one of the observation centers of the International Federation of Head and Neck Oncologic Society (IFHNOS) fellowship program from 2014. We accepted four head and neck doctors from overseas countries.
Future prospects
Transoral resection by ELPS has become one of the standard surgical procedures for early pharyngeal cancer. We are operating the prospective clinical study (TOS-J trial) to evaluate the efficacy of transoral resection for superficial pharyngeal cancer. Transoral robotic surgery (TORS) will be one of the alternatives for early hypopharyngeal and oropharyngeal carcinoma in the near future.
List of papers published in January 2017 - March 2018
Journal
1. Shinozaki T, Ebihara M, Iwase S, Yamaguchi T, Hirakawa H, Shimbashi W, Kamijo T, Okamoto M, Beppu T, Ohori J, Matsuura K, Suzuki M, Nishino H, Sato Y, Ishiki H. Quality of life and functional status of terminally ill head and neck cancer patients: a nation-wide, prospective observational study at tertiary cancer centers in Japan. Jpn J Clin Oncol, 47:47-53, 2017
2. Nishi H, Shinozaki T, Tomioka T, Maruo T, Hayashi R. Squamous cell carcinoma of the retromolar trigone: Treatment outcomes. Auris Nasus Larynx, 45:337-342, 2018