Annual Report 2017
Department of Plastic and Reconstructive Surgery
Takuya Higashino, Azusa Oshima, Yutaka Fukunaga, Yu Hokazono, Taga Marie
Introduction
The Department of Plastic and Reconstructive Surgery has mainly focused on surgical reconstruction following cancer ablation. In our institution, reconstructive procedures using free flap transfer with microvascular anastomosis are the most important operations. In addition, several methods such as tissue transfer with pedicled flaps, local flaps, and skin grafting are used for reconstructive surgery. The objectives of reconstructive surgery are not only the morphological reconstruction, but also the restoration of postoperative functions after ablative surgery. The quality of life (QOL) of patients can be improved with functional and morphological reconstruction.
Our team and what we do
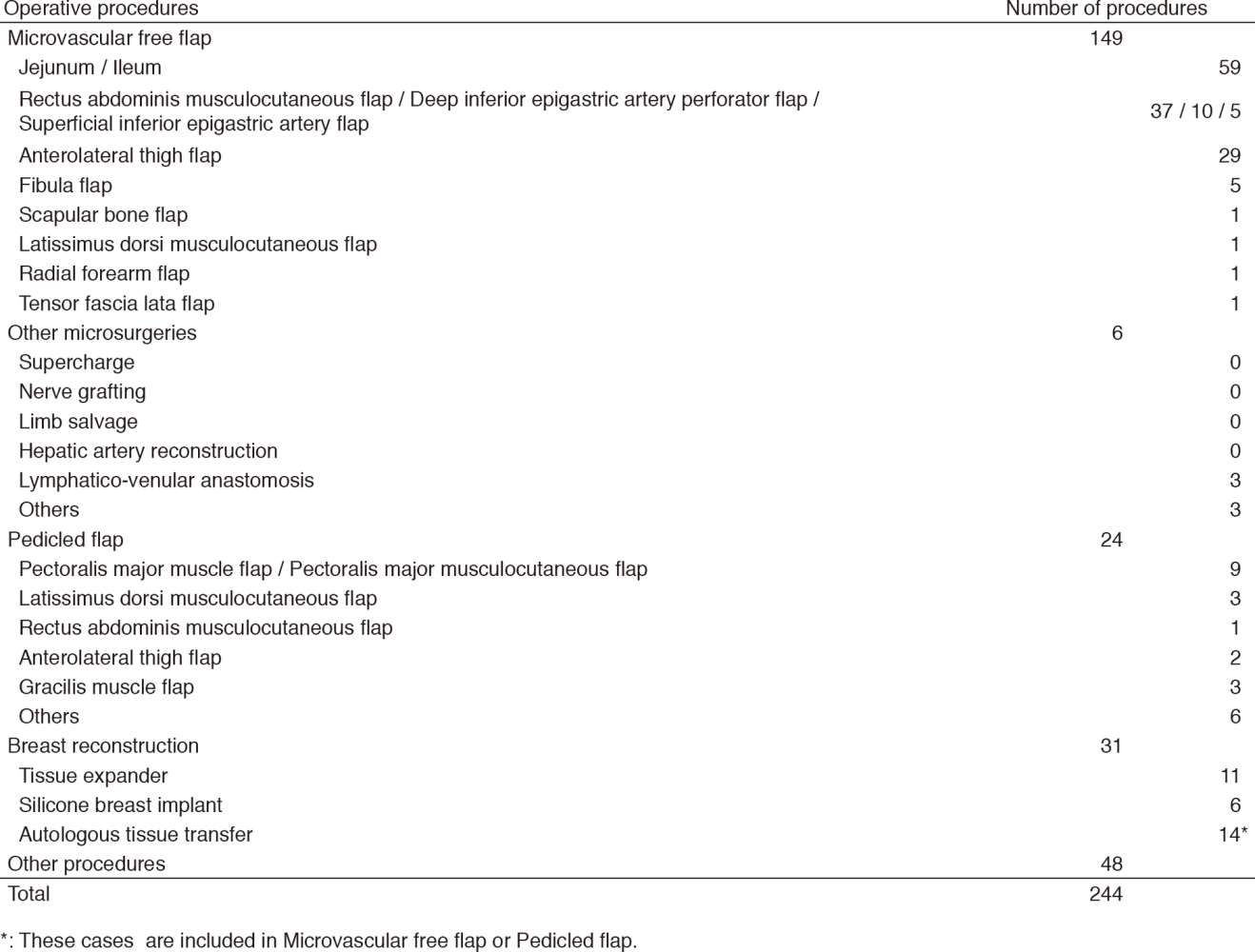
Six plastic surgeons cover reconstructive operations both in the National Cancer Center Hospital (NCCH) East in Kashiwa and the NCCH in Tokyo, in which residents are trained in both hospitals. The reconstructive surgeries are performed in cooperation with surgeons of other departments within the hospital, such as the Department of Head and Neck Surgery, Breast Surgery, Esophageal Surgery, Thoracic Surgery, Colorectal Surgery, and Urology (Table 1). In the NCCH East, head and neck reconstruction is the most frequently performed operation accounting for about 60% of the reconstructive surgeries. In the head and neck region, a free jejunal transfer and rectus abdominis musculocutaneous flap transfer are the most frequently used procedures (Table 2). A weekly conference is held with doctors of the Department of Head and Neck surgery, Radiation Oncology, and Head and Neck Medical Oncology. Breast re- construction using autologous tissue transfer was employed in 2003, since then, patients' needs for breast reconstruction is increasing. Furthermore, lymphatico-venular anastomosis as a surgical treatment for lymphedema of the extremities was introduced in 2013.
Research activities
Plastic and reconstructive surgery has focused on the following four aspects in the surgical treatment of cancer for the purpose of contributing to the improvement of the QOL of patients.
1) Obtaining good functional recovery
2) Reduction of postoperative complications
3) Achieving less donor site morbidity
4) Treatment of postoperative complications after cancer ablation
With the objective of addressing these four aspects establishing, a standard for reconstructive surgery and developing new techniques of reconstructive surgery are the most important aims of our studies. Multi-institutional analysis of postoperative complication and swallowing function after total pharyngo-laryngo-esophagectomy and reconstruction with a free jejunal transfer, in which we have took and active part, has been completed, and the result of the study was published in the journal "Plastic and Reconstructive Surgery - Global Open" in 2017. This study was supported by a Grant in-Aid for Cancer Research. The aim of the study is to clarify the relationship between surgical procedures and postoperative complications and functions.
In 2017, we also started to take an active part in a new multi-institutional analysis of risk factors for functional outcomes after tongue reconstruction.
Table 1. Number of patients (January 2017 - March 2018)
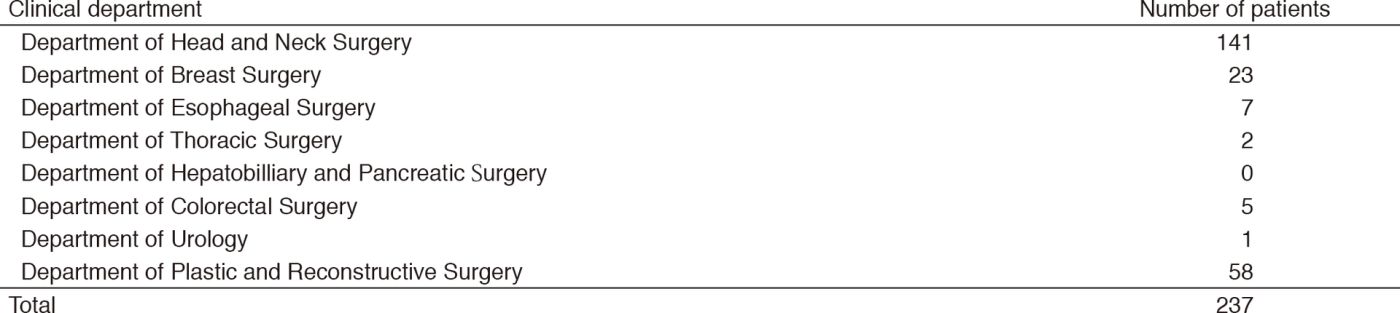
Table 2. Operative procedures (January 2017 - March 2018)
Education
We accept a lot of young plastic surgeons from all over Japan as residents and train them to become reconstructive surgeons. We also train them to become future opinion leaders in the field of reconstructive surgery.
Future prospects
The promotion of multi-institutional studies concerning reconstructive surgery will provide our patients with high-precision medical services based on evidence.
List of papers published in January 2017 - March 2018
Journal
1. Arikawa M, Miyamoto S, Fujiki M, Higashino T, Oshima A, Sakuraba M. Comparison of Donor Site Drainage Duration and Seroma Rate Between Latissimus Dorsi Musculocutaneous Flaps and Thoracodorsal Artery Perforator Flaps. Ann Plast Surg, 79:183-185, 2017
2. Tachibana S, Miyamoto S, Goto T, Ishida K, Iida T, Okazaki M, Yoshida S, Nomura S, Hayashi R, Sakuraba M. Efficacy of Tensed and Straight Free Jejunum Transfer for the Reduction of Postoperative Dysphagia. Plast Reconstr Surg Glob Open, 5:e1599, 2017
3. Sakuraba M, Miyamoto S, Fujiki M, Higashino T, Oshima A, Hayashi R. Analysis of functional outcomes in patients with mandible reconstruction using vascularized fibular grafts. Microsurgery, 37:101-104, 2017
4. Fukunaga Y, Izawa-Ishizawa Y, Horinouchi Y, Sairyo E, Ikeda Y, Ishizawa K, Tsuchiya K, Abe Y, Hashimoto I, Tamaki T. Topical application of nitrosonifedipine, a novel radical scavenger, ameliorates ischemic skin flap necrosis in a mouse model. Wound Repair Regen, 25:217-223, 2017
5. Sakuraba M, Umezawa H, Miyamoto S, Fujiki M, Higashino T, Oshima A, Tsuboi M. Reconstructive Surgery for Bronchopleural Fistula and Empyema: New Application of Free Fascial Patch Graft Combined with Free Flap. Plastic and reconstructive surgery. Global open, 5:e1199, 2017
