Annual Report 2017
Department of Colorectal Surgery
Masaaki Ito, Takeshi Sasaki, Yuji Nishizawa, Yuichiro Tsukada, Nobuyosi Takeshita, Koji Ikeda, Naoki Sakuyama, Yusuke Katayama, Koichiro Okada, Naoko Miura, Daichi Kitaguchi, Koji Inamori, Akihiro Kondo, Hiro Hasegawa, Ken Imaizumi, Hiroki Kato, Yasuaki Yamamoto, Takuya Shiraishi, Noriko Okada, Akemi Kawamura, Keiko Yao, Mieko Matsumoto, Yuko Tanabe
Introduction
Our main purpose is to contribute not only to the establishment of effective operative techniques but also to an oncological consensus including a consensus on the quality of life (QOL) and various functions of patients with pelvic malignancies. New surgical procedures, such as nerve-sparing surgery, sphincter-saving surgery, bladder-sparing surgery, pouch surgery, and minimally invasive surgery are being developed to prevent postoperative dysfunctions. These new approaches will contribute to better curability and QOL among patients with pelvic malignancies.
Our team and what we do
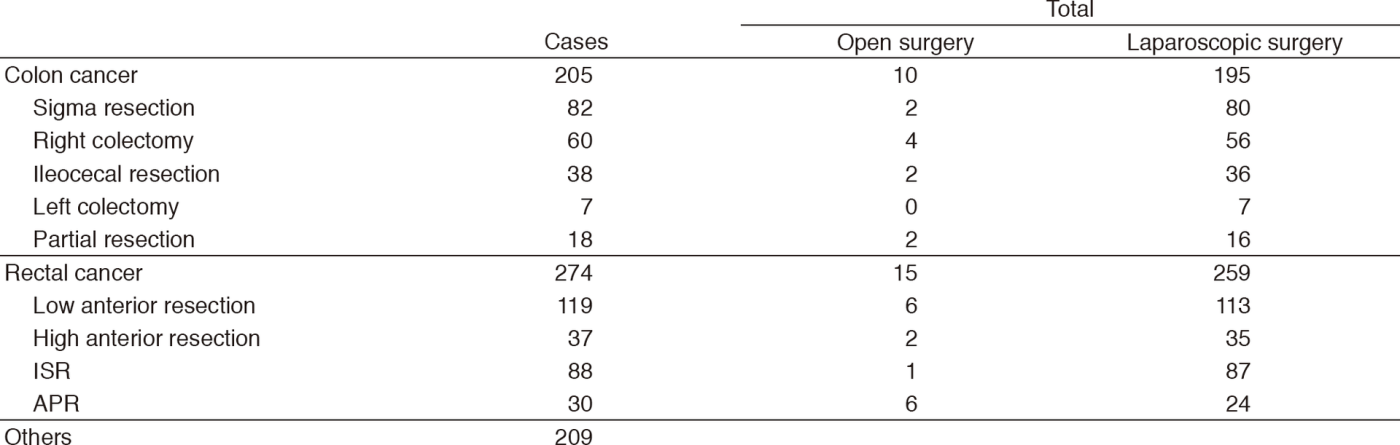
The Department of Colorectal Surgery comprises six consultants (four colorectal surgeons and two urologists) and 13 residents. The outpatient clinic is open five days a week. More than 400 new patients with colorectal carcinomas visited our department during the period from January 2017 to March 2018. Treatment plans are discussed at a weekly conference on GI malignancies and at another weekly conference on pelvic malignancies. Many treatment modalities, such as local excision with or without adjuvant chemo- or radiotherapy and other minimally invasive forms of surgery using laparoscopy, have been introduced for treatment of patients in the early stage of cancer. Laparoscopy-assisted operations (Lap-Ops) with wider lymphadenectomy of up to more than D2 are also increasingly being performed in patients with advanced colorectal carcinomas. Abdominoperineal resection (APR) has, in the past, been the standard surgery in patients with very low rectal cancer; however, partial anal sphincter preserving surgery such as intersphincteric resection (ISR) and direct CAA has been performed in more than 500 patients with very low rectal tumors and has resulted in cure, preservation of anal function, and better QOL.
Table 1. A number of surgical cases from January 2017 to March 2018
Research activities
1. Intersphincteric resection with or without neoadjuvant mFOLFOX6 study (NAIR Study)- A prospective multi-center trial -A Phase II/III randomized multicenter trial of intersphincteric resection (ISR) with or without preoperative chemotherapy for very low-lying rectal cancer
APR has been the standard surgery for very low rectal cancer located within 5 cm of the anal verge. However, a permanent colostomy causes severe impairment of QOL. This study was designed to evaluate the feasibility and the oncological and functional outcomes of ISR for very low rectal cancer. Curability with ISR was verified histologically, and acceptable oncological and functional outcomes were obtained in many patients. However, patients need to be informed preoperatively regarding the potential functional adverse effects after ISR. This study is in progress, and 50 patients have been registered.
2. Bladder-sparing surgery for locally advanced rectal cancer involving the prostate
Total pelvic exenteration (TPE) is the standard procedure in such patients. This study aims to evaluate the feasibility of bladder-sparing surgery as an alternative to TPE. This procedure has been performed in 39 patients with primary or recurrent tumors and permits conservative surgery in selected patients with advanced rectal cancer involving the prostate without compromising local control.
3. A prospective randomized trial for the feasibility and effect of lateral node dissection in low rectal cancer ‐ (Total) Mesorectal Excision (ME) vs. Lateral Node Dissection with preservation of autonomic nerves (D3 with nerve-sparing) [JCOG0212 CRC Surg.]
In this study, 76 patients have been registered.
4. Local excision with postoperative chemoradiotherapy for T1hT2 rectal cancer
This study aims to evaluate preoperatively the feasibility and oncologic outcomes of local therapy for T1 and a part of T2 rectal cancer without lymph node metastases. In this study, 82 patients have been registered.
5. Study on Robotic surgery for rectal cancer
This study is closed.
Clinical trials
Other clinical trials are also in progress as follows.
- A Phase I/II trial of chemoradiotherapy concurrent with S-1 plus MMC in patients with clinical stage II/III squamous cell carcinoma of the anal canal (JCOG0903)
- A randomized study of conventional technique vs. no-touch isolation technique (JCOG1006)
- A randomized controlled trial comparing resection of primary tumor plus chemotherapy with chemotherapy alone in incurable Stage IV colorectal cancer (JCOG1007)
- A randomized Phase III study of mFOLFOX7 or CAPOX plus bevacizumab versus 5-fluorouracil/leucovorin or capecitabine plus bevacizumab as first-line treatment in elderly patients with metastatic colorectal cancer (JCOG1018)
- A randomized controlled trial comparing laparoscopic surgery with open surgery in palliative resection of primary tumor in incurable Stage IV colorectal cancer (JCOG1107)
- A Prospective Phase II Trial of Laparoscopic Surgery for Ultra-low Rectal Cancers within Five Centimeters from the Anus or Three Centimeters from the Dentate Line. Under the Japanese Society for Cancer of the Colon and Rectum (JSCCR)
- A prospective study of urinary and sexual dysfunction after surgery for rectal cancer
- A Phase II study of neoadjuvant mFOLFOX6 (+ cetuximab) in patients with resectable pelvic recurrences after rectal cancer surgery
- Development of LAP-instruments for colorectal surgery
- A Phase II study of usage of new anal tube following TME for rectal cancer
Education
1) Guiding university students in their studies
2) Guiding colorectal surgeons for becoming medical specialists
3) Holding a taTME seminar for Japanese surgeons as a training of taTME procedures
Future prospects
The establishment of less-invasive surgery for cure and function-preserving in cancer patients with colorectal malignancies is our goal.
List of papers published in January 2017 - March 2018
Journal
1. Sakai Y, Komai Y, Saito N, Ito M, Sakuraba M. Analysis of a Surgical Treatment for Persistent Urorectal Fistulas after Radical Cancer Surgery: A Comparison of Prostate Cancer and Rectal Cancer. Urol Int, 99:56-62, 2017
2. Nishigori H, Ito M, Nishizawa Y. A novel transanal tube designed to prevent anastomotic leakage after rectal cancer surgery: the WING DRAIN. Surg Today, 47:513-520, 2017
3. Noguchi K, Nishizawa Y, Komai Y, Sakai Y, Kobayasi A, Ito M, Saito N. Efficacy of an additional flap operation in bladder-preserving surgery with radical prostatectomy and cystourethral anastomosis for rectal cancer involving the prostate. Surg Today, 47:1119-1128, 2017
4. Yamamoto S, Hinoi T, Niitsu H, Okajima M, Ide Y, Murata K, Akamoto S, Kanazawa A, Nakanishi M, Naitoh T, Kanehira E, Shimamura T, Suzuka I, Fukunaga Y, Yamaguchi T, Watanabe M. Influence of previous abdominal surgery on surgical outcomes between laparoscopic and open surgery in elderly patients with colorectal cancer: subanalysis of a large multicenter study in Japan. J Gastroenterol, 52:695-704, 2017
5. Tanaka K, Okuda J, Yamamoto S, Ito M, Sakamoto K, Kokuba Y, Yoshimura K, Watanabe M. Risk factors for anastomotic leakage after laparoscopic surgery with the double stapling technique for stage 0/I rectal carcinoma: a subgroup analysis of a multicenter, single-arm phase II trial. Surg Today, 47:1215-1222, 2017
6. Fujita S, Mizusawa J, Kanemitsu Y, Ito M, Kinugasa Y, Komori K, Ohue M, Ota M, Akazai Y, Shiozawa M, Yamaguchi T, Bandou H, Katsumata K, Murata K, Akagi Y, Takiguchi N, Saida Y, Nakamura K, Fukuda H, Akasu T, Moriya Y. Mesorectal Excision With or Without Lateral Lymph Node Dissection for Clinical Stage II/III Lower Rectal Cancer (JCOG0212): A Multicenter, Randomized Controlled, Noninferiority Trial. Ann Surg, 266:201-207, 2017
7. Yokota M, Ito M, Nishizawa Y, Kobayashi A, Saito N. The Impact of Anastomotic Leakage on Anal Function Following Intersphincteric Resection. World J Surg, 41:2168-2177, 2017
8. Matsunaga R, Nishizawa Y, Saito N, Kobayashi A, Ohdaira T, Ito M. Quantitative evaluation of 3D imaging in laparoscopic surgery. Surg Today, 47:440-444, 2017
9. Matsunaga R, Nishizawa Y, Saito N, Yokota M, Hayashi R, Ito M. Anal Function after Surgery for Low-Lying Rectal Cancer: Comparison of Mechanical and Hand-Sewn Coloanal Anastomosis. Dig Surg, 34:469-475, 2017
10. Kitano S, Inomata M, Mizusawa J, Katayama H, Watanabe M, Yamamoto S, Ito M, Saito S, Fujii S, Konishi F, Saida Y, Hasegawa H, Akagi T, Sugihara K, Yamaguchi T, Masaki T, Fukunaga Y, Murata K, Okajima M, Moriya Y, Shimada Y. Survival outcomes following laparoscopic versus open D3 dissection for stage II or III colon cancer (JCOG0404): a phase 3, randomised controlled trial. The lancet. Gastroenterology & hepatology, 2:261-268, 2017
11. Sasaki T, Ito Y, Ohue M, Kanemitsu Y, Kobatake T, Ito M, Moriya Y, Saito N. Postoperative Chemoradiotherapy After Local Resection for High-Risk T1 to T2 Low Rectal Cancer: Results of a Single-Arm, Multi-Institutional, Phase II Clinical Trial. Dis Colon Rectum, 60:914-921, 2017
12. Yamaguchi T, Konishi T, Kinugasa Y, Yamamoto S, Akiyoshi T, Okamura R, Ito M, Nishimura Y, Shiozawa M, Yamaguchi S, Hida K, Sakai Y, Watanabe M. Laparoscopic Versus Open Lateral Lymph Node Dissection for Locally Advanced Low Rectal Cancer: A Subgroup Analysis of a Large Multicenter Cohort Study in Japan. Dis Colon Rectum, 60:954-964, 2017
13. Yamazaki N, Koga Y, Taniguchi H, Kojima M, Kanemitsu Y, Saito N, Matsumura Y. High expression of miR-181c as a predictive marker of recurrence in stage II colorectal cancer. Oncotarget, 8:6970-6983, 2017
14. Kawai T, Hayashi H, Nishizawa Y, Nishikawa A, Nakamura R, Kawahira H, Ito M, Nakamura T. Compact forceps manipulator with a spherical-coordinate linear and circular telescopic rail mechanism for endoscopic surgery. Int J Comput Assist Radiol Surg, 12:1345-1353, 2017
15. Hamabe A, Ito M. A three-dimensional pelvic model made with a three-dimensional printer: applications for laparoscopic surgery to treat rectal cancer. Tech Coloproctol, 21:383-387, 2017
16. Sakuyama N, Kojima M, Kawano S, Matsuda Y, Mino-Kenudson M, Ochiai A, Ito M. Area of residual tumor is a robust prognostic marker for patients with rectal cancer undergoing preoperative therapy. Cancer Sci, 109:871-878, 2018
17. Hoshino N, Hida K, Sakai Y, Osada S, Idani H, Sato T, Takii Y, Bando H, Shiomi A, Saito N. Nomogram for predicting anastomotic leakage after low anterior resection for rectal cancer. Int J Colorectal Dis, 33:411-418, 2018
18. Ito M, Kobayashi A, Fujita S, Mizusawa J, Kanemitsu Y, Kinugasa Y, Komori K, Ohue M, Ota M, Akazai Y, Shiozawa M, Yamaguchi T, Akasu T, Moriya Y. Urinary dysfunction after rectal cancer surgery: Results from a randomized trial comparing mesorectal excision with and without lateral lymph node dissection for clinical stage II or III lower rectal cancer (Japan Clinical Oncology Group Study, JCOG0212). Eur J Surg Oncol, 44:463-468, 2018
19. Hamabe A, Ito M, Nishigori H, Nishizawa Y, Sasaki T. Preventive effect of diverting stoma on anastomotic leakage after laparoscopic low anterior resection with double stapling technique reconstruction applied based on risk stratification. Asian J Endosc Surg, 11:220-226, 2018
20. Kochi M, Hinoi T, Niitsu H, Ohdan H, Konishi F, Kinugasa Y, Kobatake T, Ito M, Inomata M, Yatsuoka T, Ueki T, Tashiro J, Yamaguchi S, Watanabe M. Risk factors for postoperative pneumonia in elderly patients with colorectal cancer: a sub-analysis of a large, multicenter, case-control study in Japan . Surg Today, 48:756-764, 2018
21. Imaizumi K, Nishizawa Y, Ikeda K, Tsukada Y, Sasaki T, Ito M. Extended pelvic resection for rectal and anal canal tumors is a significant risk factor for perineal wound infection: a retrospective cohort study. Surg Today, 2018
22. Kitaguchi D, Nishizawa Y, Sasaki T, Tsukada Y, Kondo A, Hasegawa H, Ito M. A Rare Complication After Laparoscopic Lateral Lymph Node Dissection for Rectal Cancer: Two Case Reports of Internal Hernia Below the Superior Vesical Artery. Journal of the Anus, Rectum and Colon(JARC), 2:110-114, 2018
Book
1. Ito M. Transanal Total Mesorectal Excision. In: Kim NK, Sugihara K, Liang JT (eds), Surgical Treatment of Colorectal Cancer Asian Perspectives on Optimization and Standardization, pp 209-219, 2018