Annual Report 2017
Department of Neurosurgery and Neuro-Oncology
Yoshitaka Narita, Yasuji Miyakita, Makoto Ohno, Masamichi Takahashi, Takahiro Yamauchi, Natsuko Tsushita, Erika Yamazawa
Introduction
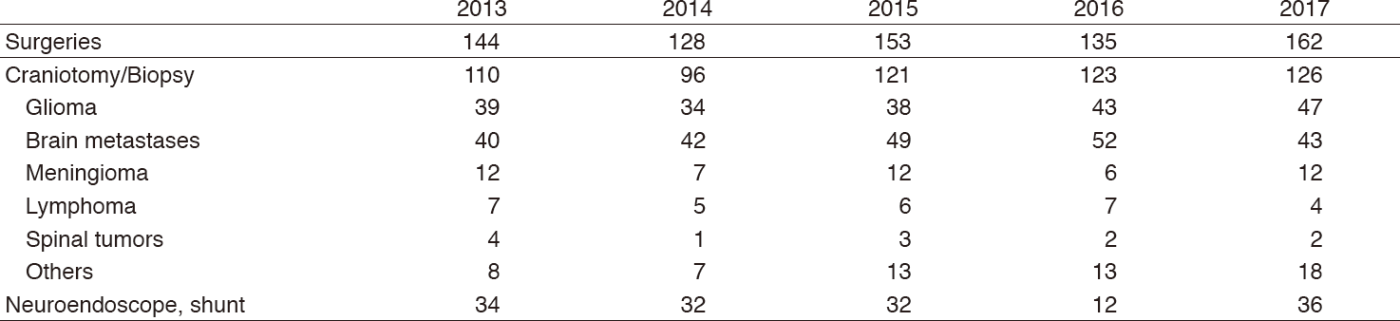
We treat patients with primary and metastatic brain tumors. Approximately 300 patients were admitted and 126 craniotomies for tumor removal were carried out in 2017 including 47 gliomas, 43 brain metastases, four primary central nervous system (CNS) lymphomas, and 12 meningiomas (Table 1). The site of the craniotomy and the extent of tumor removal were visualized on the intraoperative magnetic resonance imaging (MRI) in real time, contributing to safer and more precise surgery. Intraoperative monitoring with motor- and sensory-evoked potential (MEP and SEP) recording as well as preoperative functional MRI and magnetic resonance (MR) tractography were also used to preserve patient neurological function. Awake surgeries were also performed, particularly for the removal of gliomas near the speech center. Patients with malignant brain tumors were treated with postoperative radiotherapy and chemotherapy. In order to design a more effective chemotherapy regimen, molecular biological studies for drug resistance, growth factors, cell kinetic studies on individual tumors, and several clinical trials are ongoing.
Our team and what we do
A weekly conference on the treatment of patients with brain tumors is held with doctors of the Department of Radiation Oncology of the National Cancer Center Hospital (NCCH) and the Division of Brain Tumor Translational Research of the NCC Research Institute (NCCRI). Usually 15-20 patients are hospitalized and two or three of them undergo surgical treatment every week. Patients with malignant brain tumors receive postoperative radiotherapy and chemotherapy. Statistical analysis revealed that surgical removal of as much of the tumor as possible yielded better survival rates even for the most malignant glioblastomas, which usually recur soon after the surgery without radiotherapy. Concomitant use of chemotherapy is considered to enhance the anti-tumor effect of radiotherapy. Temozolomide has been given to all malignant glioma patients during radiotherapy and repeated every month for two years. High dose methotrexate is administered to the patients with primary CNS lymphoma before radiotherapy.
Table 1 Number of surgical cases
The decision on the indication for surgery of metastatic brain tumors is not simple. Multiplicity of brain metastasis, the stage of the primary malignancy, and the patient performance status should be taken into careful consideration.
Research activities
Patients with brain tumors have been registered in the Brain Tumor Registry of Japan (BTRJ) since 1969. More than 100,000 patients have been registered and followed up. The Department of Neurosurgery and Neuro-Oncology of the NCCH contributes as a managing office of the BTRJ and established on-line registration using the University Hospital Medical Information Network (UMIN) system in 2009. Clinical data during 2005 and 2008 were collected and the report was published in 2017 as a supplement of the official journal of the Japan Neurosurgical Society.
An analysis of gene expression profiles in malignant gliomas is being carried out in order to determine specific genes that have an influence on the effects of chemotherapy and radiation therapy in cooperation with the Division of Brain Tumor Translational Research of the NCCRI. The determination of the methylation status of O6-methylguanine-DNA methyltransferase (MGMT) and the mutation of IDH1/2 and telomerase reverse transcriptase (TERT) are also carried out to predict the prognosis of the patients with malignant gliomas.
Clinical trials
The Japan Clinical Oncology Group (JCOG)-Brain Tumor Study Group (BTSG) was organized in 2002 and a multi-institutional randomized controlled trial is performed. "A Randomized phase III trial of postoperative whole brain radiation therapy compared with salvage stereotactic radiosurgery in patients with one to four brain metastasis (JCOG0504)" was finished and presented in ASCO2017 meeting. "Phase III randomized Study in patients with anaplastic glioma of radiotherapy with versus nimustine hydrochloride (ACNU) followed by temozolomide (JCOG1016)", "Phase III Study of High-dose Methotrexate and Whole Brain Radiotherapy With or Without Concomitant and Adjuvant Temozolomide in Patients with Primary CNS Lymphoma (JCGO1114)", "Randomized phase III study for unresectable WHO Grade II astrocytoma with radiotherapy alone or chemoradiotherapy with temozolomide (JCOG1303)", and "multicenter randomized phase III study for recurrent glioblastoma comparing bevacizumab alone with dose-dense temozolomide followed by bevacizumab (JCOG1308)" are now ongoing. These studies, under the surveillance of the JCOG, aim to set a standard protocol for treating malignant brain tumor patients. Moreover, a proper methodology for performing randomized studies will be established in the field of neuro-oncology.
An Investigator-initiated phase II clinical trial of eribulin targeting TERT in patients with recurrent glioblastomas has been started.
Education
Our department plays the roles of the office of the general secretary of the JCOG-BTSG and BTRJ; we conducted many clinical trials and brain tumor registries. We educate many neurosurgeons and oncologists about surgical techniques of awake craniotomy and intraoperative MRI and the effective usage and adverse effects of many chemotherapeutic agents about malignant brain tumors.
Future prospects
Malignant brain tumors, especially glioblastoma, still have the worse prognosis among cancers. We always make an effort to defeat these brain cancers through various clinical works and research.
List of papers published in January 2017 - March 2018
Journal
1.Aihara K, Mukasa A, Nagae G, Nomura M, Yamamoto S, Ueda H, Tatsuno K, Shibahara J, Takahashi M, Momose T, Tanaka S, Takayanagi S, Yanagisawa S, Nejo T, Takahashi S, Omata M, Otani R, Saito K, Narita Y, Nagane M, Nishikawa R, Ueki K, Aburatani H, Saito N. Genetic and epigenetic stability of oligodendrogliomas at recurrence. Acta neuropathologica communications, 5:18, 2017
2.Nakamura T, Yamashita S, Fukumura K, Nakabayashi J, Tanaka K, Tamura K, Tateishi K, Kinoshita M, Fukushima S, Takami H, Fukuoka K, Yamazaki K, Matsushita Y, Ohno M, Miyakita Y, Shibui S, Kubo A, Shuto T, Kocialkowski S, Yamanaka S, Mukasa A, Sasayama T, Mishima K, Maehara T, Kawahara N, Nagane M, Narita Y, Mano H, Ushijima T, Ichimura K. Genome-wide DNA methylation profiling identifies primary central nervous system lymphoma as a distinct entity different from systemic diffuse large B-cell lymphoma. Acta Neuropathol, 133:321-324, 2017
3.Fukushima S, Yamashita S, Kobayashi H, Takami H, Fukuoka K, Nakamura T, Yamasaki K, Matsushita Y, Nakamura H, Totoki Y, Kato M, Suzuki T, Mishima K, Yanagisawa T, Mukasa A, Saito N, Kanamori M, Kumabe T, Tominaga T, Nagane M, Iuchi T, Yoshimoto K, Mizoguchi M, Tamura K, Sakai K, Sugiyama K, Nakada M, Yokogami K, Takeshima H, Kanemura Y, Matsuda M, Matsumura A, Kurozumi K, Ueki K, Nonaka M, Asai A, Kawahara N, Hirose Y, Takayama T, Nakazato Y, Narita Y, Shibata T, Matsutani M, Ushijima T, Nishikawa R, Ichimura K. Genome-wide methylation profiles in primary intracranial germ cell tumors indicate a primordial germ cell origin for germinomas. Acta Neuropathol, 133:445-462, 2017
4.Brain Tumor Registry of Japan (2005-2008). Neurol Med Chir (Tokyo), 57:9-102, 2017
5.Nomura M, Mukasa A, Nagae G, Yamamoto S, Tatsuno K, Ueda H, Fukuda S, Umeda T, Suzuki T, Otani R, Kobayashi K, Maruyama T, Tanaka S, Takayanagi S, Nejo T, Takahashi S, Ichimura K, Nakamura T, Muragaki Y, Narita Y, Nagane M, Ueki K, Nishikawa R, Shibahara J, Aburatani H, Saito N. Distinct molecular profile of diffuse cerebellar gliomas. Acta Neuropathol, 134:941-956, 2017
6.Katanoda K, Shibata A, Matsuda T, Hori M, Nakata K, Narita Y, Ogawa C, Munakata W, Kawai A, Nishimoto H. Childhood, adolescent and young adult cancer incidence in Japan in 2009-2011. Jpn J Clin Oncol, 47:762-771, 2017
7.Kuramoto K, Suzuki S, Sakaki H, Takeda H, Sanomachi T, Seino S, Narita Y, Kayama T, Kitanaka C, Okada M. Licochalcone A specifically induces cell death in glioma stem cells via mitochondrial dysfunction. FEBS open bio, 7:835-844, 2017
8.Narita Y. Chemotherapy of Diffuse Astrocytoma (WHO grade II) in Adults. Prog Neurol Surg, 31:145-151, 2018
9.Miki S, Imamichi S, Fujimori H, Tomiyama A, Fujimoto K, Satomi K, Matsushita Y, Matsuzaki S, Takahashi M, Ishikawa E, Yamamoto T, Matsumura A, Mukasa A, Nishikawa R, Masutomi K, Narita Y, Masutani M, Ichimura K. Concomitant administration of radiation with eribulin improves the survival of mice harboring intracerebral glioblastoma. Cancer Sci, 109:2275-2285, 2018
10.Yamamoto Y, Sasaki N, Kumagai K, Takeuchi S, Toyooka T, Otani N, Wada K, Narita Y, Ichimura K, Namba H, Mori K, Tomiyama A. Involvement of Intracellular Cholesterol in Temozolomide-Induced Glioblastoma Cell Death. Neurol Med Chir (Tokyo), 58:296-302, 2018
11.Yamamoto Y, Tomiyama A, Sasaki N, Yamaguchi H, Shirakihara T, Nakashima K, Kumagai K, Takeuchi S, Toyooka T, Otani N, Wada K, Narita Y, Ichimura K, Sakai R, Namba H, Mori K. Intracellular cholesterol level regulates sensitivity of glioblastoma cells against temozolomide-induced cell death by modulation of caspase-8 activation via death receptor 5-accumulation and activation in the plasma membrane lipid raft. Biochem Biophys Res Commun, 495:1292-1299, 2018