Annual Report 2017
Department of Head and Neck Oncology
Seiichi Yoshimoto, Fumihiko Matsumoto, Go Omura, Kenya Kobayashi, Satoko Matsumura, Masahiko Fukazawa, Yoshifumi Matsumoto, Ayaka Mori
Introduction
The treatment strategy for head and neck cancer is to improve the survival rate while preserving significant functions including speech, mastication, swallowing and cosmetic appearance. In order to achieve this strategy, the Department of Head and Neck Oncology has tried to select the best treatment modality and devise new surgical procedures based on clinic-pathological findings and our large database of patients with head and neck cancer.
Our department has developed and performed original surgical procedures of partial or subtotal laryngectomy for newly-diagnosed and radiation-failed laryngeal cancer, partial pharyngectomy for hypopharyngeal cancer, and total glossectomy for advanced tongue cancer. These surgical approaches can be performed without sacrificing the larynx. Compared with the results of conventional surgery, there are apparently fewer wound complications. Patients can resume social activities more easily when they maintain their ability to communicate vocally.
Our team and what we do
The Department of Head and Neck Oncology at the NCCH consists of eight head and neck surgeons. Many operations are performed under general and local anesthesia with or without microsurgical reconstructive surgery. In addition to radiotherapy, concurrent chemo-radiotherapy is performed with the Department of Radiation Oncology.
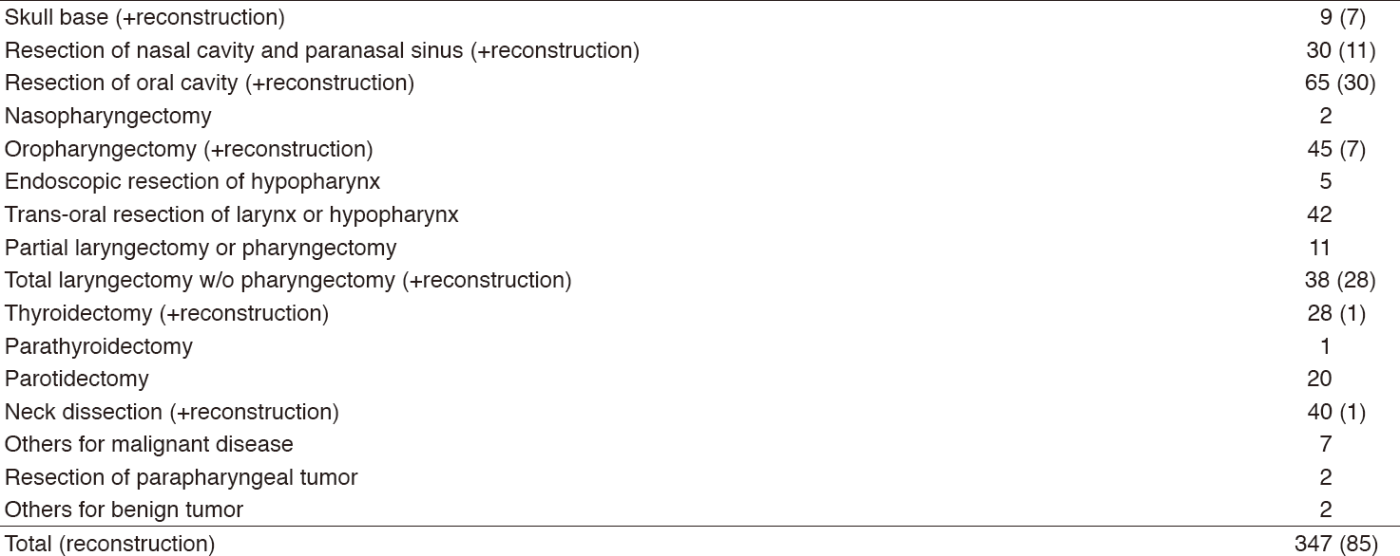
In 2017, 464 patients with head and neck tumor underwent surgery under local or general anesthesia; 117 and 347, respectively, including 85 patients with major ablation and free flap reconstructive surgery. Table 1 shows the number of surgical cases under general anesthesia.
Research activities
We have been taking part in multi-institutional studies of sentinel lymph node navigation surgery for oral cavity cancer using RI and laryngopharyngeal cancer using ICG. We are also taking part in JCOG (Japanese Clinical Oncology Group) study concerning postoperative chemoradiotherapy and intra-arterial chemoradiotherapy for maxillary sinus cancer.
Clinical trials
We are participating in a few clinical trials about immune checkpoint inhibitors and BNCT (Boron Neutron Capture Therapy).
Education
We provide plenty of educational opportunities for resident doctors, especially focusing on acquiring operative techniques. They can learn everything about perioperative management, such as physical examination, image diagnosis, informed consent, preoperative preparation and postoperative management.
Future prospects
Trans-oral resection for superficial laryngo-
pharyngeal cancer will be indicated for more patients. The number of patients with HPV-elated oropharyngeal cancer has increased. Treatment strategy for this disease should be discussed. Immune checkpoint inhibitors are used for chemo-
resistant patients with recurrent or metastatic tumor. We will be able to get useful information about the response rate of these drugs for Japanese patients.
List of papers published in January 2017 - March 2018
Journal
1. Maki D, Mori T, Teshima M, Kobayashi K, Matsumoto F, Sakai A, Okami K, Yoshimoto S. Chondrosarcoma of the hyoid bone - Report of a case and a literature review of the suitable treatment strategy. Auris Nasus Larynx, 44:629-634, 2017
2. Miura K, Hirakawa H, Uemura H, Yoshimoto S, Shiotani A, Sugasawa M, Homma A, Yokoyama J, Tsukahara K, Yoshizaki T, Yatabe Y, Matsuo K, Ohkura Y, Kosuda S, Hasegawa Y. Sentinel node biopsy for oral cancer: A prospective multicenter Phase II trial. Auris Nasus Larynx, 44:319-326, 2017
3. Matsumoto F, Mori T, Matsumura S, Matsumoto Y, Fukasawa M, Teshima M, Kobayashi K, Yoshimoto S. Prognostic significance of surgical extranodal extension in head and neck squamous cell carcinoma patients. Jpn J Clin Oncol, 47:699-704, 2017
4. Kobayashi K, Mori T, Matsumoto F, Murakami N, Teshima M, Fukasawa M, Matsumoto Y, Matsumura S, Itami J, Asai M, Yoshimoto S. Impact of microscopic orbital periosteum invasion in orbital preservation surgery. Jpn J Clin Oncol, 47:321-327, 2017
