Annual Report 2017
Department of Breast Surgery
Takayuki Kinoshita, Shin Takayama, Sota Asaga, Kenjiro Jimbo, Sho Shiino, Toshiaki Kurihara, Eriko Iwamoto
Introduction
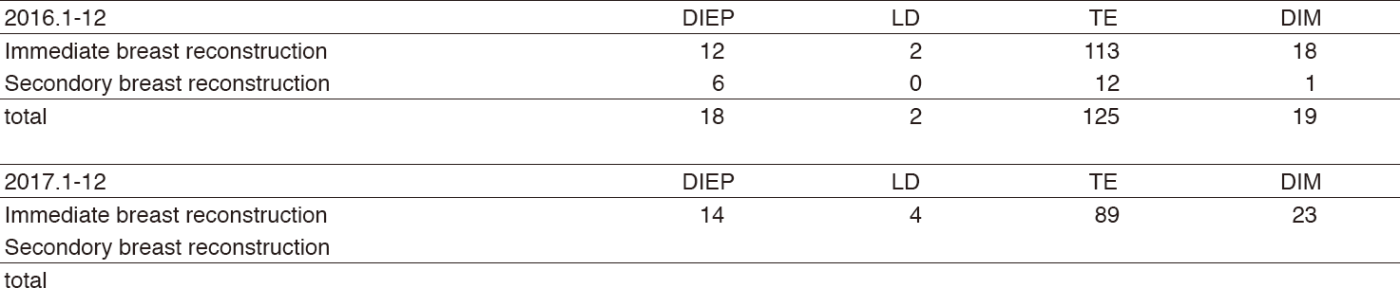
The Department of Breast Surgery deals with treatment of breast cancer through surgeries, as well as diagnosis of breast diseases and assessment of lymph nodes in the axillary and clavicular regions which are suspected harboring metastases. The trend of surgical procedure has been changing year by year. Although breast partial resection (Bp) accounted for 38% of the total surgeries in our department in 2017, Bp is on the decline in recent years. One of the reasons is the increasing needs of immediate reconstruction surgeries. In our hospital, since 2010, immediate breast reconstruction became one of the choices for patients in whom breast preservation was cosmetically difficult, and a total of 130 immediate breast reconstructions were performed in 2017, comprising 18% of all cases. Eighty-nine out of 130 were tissue expander (TE) and 23 direct implant (DIM), and 18 autologous reconstruction (14 DIEP; deep inferior epigastric perforator flap, and four LD; latissimus dorsi muscle flap) were done. We perform these reconstruction surgeries in cooperation with plastic surgeons depending on patients' needs. And the new less invasive technique, radiofrequency abrasion (RFA), is another reason. In 2017, 34 RFAs were performed. The number of cases of immediate breast reconstruction has increased year by year to match increasing needs of patients. Sentinel lymph node (SLN) biopsies (SLNB) were performed in 81% of cases. Following SLNB, the axillary lymph node dissection (ALND) could be avoided when the SLNB was negative. One-step nucleic acid amplification (OSNA) assay that quantitatively measures CK19 mRNA detects sentinel lymph node metastases even in molecular levels, and in conjunction with this assay and conventional microscopic method, we began to be able to evaluate the SLN more precisely. Further, by comparing the OSNA results with that of conventional histological diagnosis, we try to search the possibility of omitting axillary lymph node dissection by using two methods. Thus, to meet the diverse needs of breast cancer patients, we are striving continuously.
Our team and what we do
Our department comprised of six staff surgeons, one chief resident, and three or four rotating residents. From 7:15 every morning, all the staff and residents perform in patient rounds together. Journal clubs and research conferences are scheduled for every Tuesday morning after rounds. Weekly conferences are held on Monday from 17:00 to 18:30, and on Wednesday from 17:00 to 18:00 for shared discussions with surgeons, and the diagnostic images of pre-operative patients are reviewed and compared with pathological reports in every postoperative patient. A breast pathology/imaging conference is held on the second Wednesday of every two months from 19:00 to 20:00 to discuss problems with diagnostic imaging, and with pathologically interesting cases. A conference about studies, institutional treatment guidelines, and recent topics regarding breast cancer is also held irregularly by a multidisciplinary team. Treatment Guidelines for primary and metastatic breast cancer have been updated regularly through this multidisciplinary discussion since 2003.
Surgery
We perform surgeries from Monday to
Friday, regularly 15 to 18 cases of breast cancer in a week. Table 1 shows a total number of patients with primary breast cancer (including breast primary sarcoma) and other breast diseases. The types and number of operative procedures are shown in Table 2. The rate of mastectomy was 56%, including 130 cases of immediate reconstruction. SLNB was performed in 479 (81%) patients, and many patients were spared from ALND in 2017.
Research activities
1. Radiofrequency ablation therapy for early breast cancer as local therapy (RAFAELO study)
2. Intensive vs. standard post-operative surveillance in high risk breast cancer patients (JCOG1204, INSPIRE Trial)
3. Single-arm confirmatory trial of endocrine therapy alone for estrogen positive, low-risk ductal carcinoma in situ of the breast (Low-risk DCIS with endocrine therapy alone-TAM)
(JCOG1505, LORETTA Trial)
4. Denosumab adjuvant treatment (D-CARE)
5. Scalp-cooling device during chemotherapy
6. Postoperative Therapy with Endocrine and TS-1 (POTENT study)
7. Registration Data-base System of the breast cancer patient who carried out the lymph node metastasis diagnosis by the OSNA method (LynoLog Data-base)
8. Olaparib as Adjuvant Treatment in Patients With Germline BRCA Mutated High Risk HER2 Negative Primary Breast Cancer (OlympiA)
9. Hair Loss Prevention System with
chemotherapy-induced alopecia in breast cancer patients in Japan (HOPE)
Future prospects
The aims of our activities are as follows:
1. Clinical activity
To provide the very best breast surgical treatment
2. Research activity
To develop less invasive breast surgical procedure
3. Educational activity
To bring up specialists in breast cancer who lead the future of cancer fields
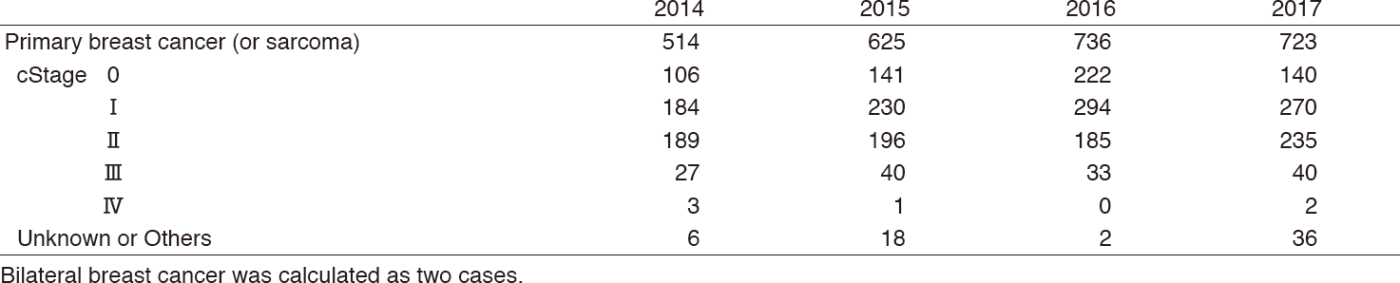
Table 2-1. Types of procedures (breast surgery)
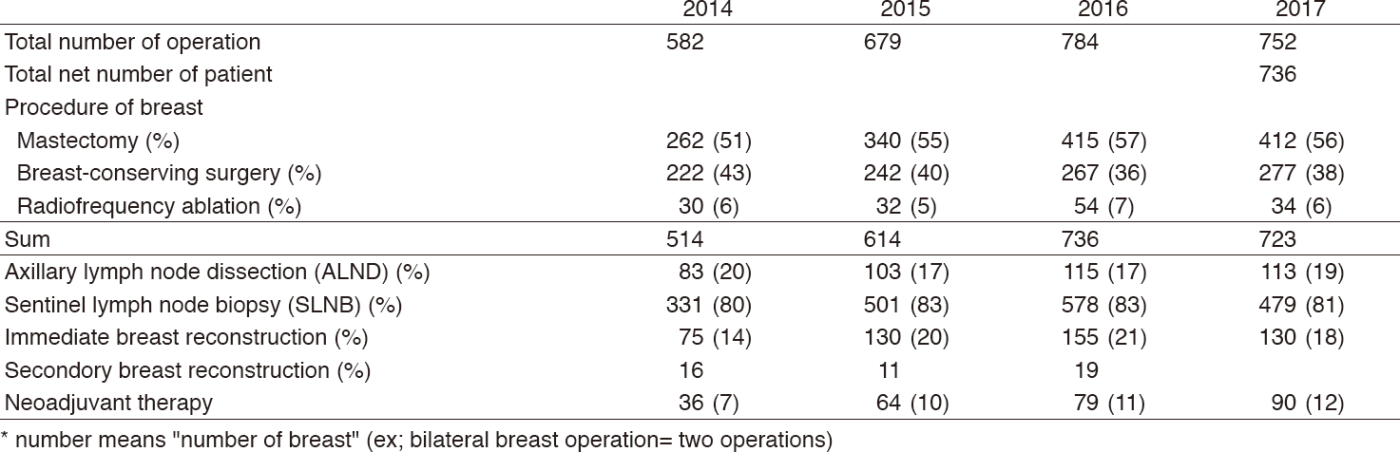
Table2-2. Types of procedures (reconstruction surgery)
List of papers published in January 2017 - March 2018
Journal
1. Ono M, Tsuda H, Yoshida M, Shimizu C, Kinoshita T, Tamura K. Prognostic Significance of Progesterone Receptor Expression in Estrogen-Receptor Positive, HER2-Negative, Node-Negative Invasive Breast Cancer With a Low Ki-67 Labeling Index. Clin Breast Cancer, 17:41-47, 2017
2. Ohara K, Arai E, Takahashi Y, Ito N, Shibuya A, Tsuta K, Kushima R, Tsuda H, Ojima H, Fujimoto H, Watanabe SI, Katai H, Kinoshita T, Shibata T, Kohno T, Kanai Y. Genes involved in development and differentiation are commonly methylated in cancers derived from multiple organs: a single-institutional methylome analysis using 1007 tissue specimens. Carcinogenesis, 38:241-251, 2017
3. Tanabe Y, Tsuda H, Yoshida M, Yunokawa M, Yonemori K, Shimizu C, Yamamoto S, Kinoshita T, Fujiwara Y, Tamura K. Pathological features of triple-negative breast cancers that showed progressive disease during neoadjuvant chemotherapy. Cancer Sci, 108:1520-1529, 2017
4. Sasada S, Kurihara H, Kinoshita T, Yoshida M, Honda N, Shimoi T, Shimomura A, Yunokawa M, Yonemori K, Shimizu C, Hamada A, Kanayama Y, Watanabe Y, Fujiwara Y, Tamura K. 64Cu-DOTA-trastuzumab PET imaging for HER2-specific primary lesions of breast cancer. Ann Oncol, 28:2028-2029, 2017
5. Shimoi T, Yoshida M, Kitamura Y, Yoshino T, Kawachi A, Shimomura A, Noguchi E, Yunokawa M, Yonemori K, Shimizu C, Kinoshita T, Ichimura K, Fukuda T, Fujiwara Y, Tamura K. TERT promoter hotspot mutations in breast cancer. Breast Cancer, 25:292-296, 2018
6. Mizota Y, Ohashi Y, Iwase T, Iwata H, Sawaki M, Kinoshita T, Taira N, Mukai H, Yamamoto S. Rainbow of KIBOU (ROK) study: a Breast Cancer Survivor Cohort in Japan. Breast Cancer, 25:60-67, 2018