Annual Report 2017
Department of Endoscopy, Gastrointestinal Endoscopy Division (Endoscopy Center)
Yutaka Saito, Takahisa Matsuda, Ichiro Oda, Yasuo Kakugawa, Takeshi Nakajima, Shigetaka Yoshinaga, Haruhisa Suzuki, Satoru Nonaka, Taku Sakamoto, Seiichiro Abe, Masayoshi Yamada,
Masau Sekiguchi and Hiroyuki Takamaru (Gastrointestinal Endoscopy, National Cancer Center Hospital)
Yuji Matsumoto and Takaaki Tsuchida (Bronchoscopy)
Introduction
The Department of Endoscopy moved to the New Endoscopy Center on January 20th, 2014 and we believe this is currently the biggest endoscopy center in Japan (15 Endoscopy Rooms [251.112m2] and 136.788m2 Recovery Rooms on two floors of 1949.554m2).
The total number of nursing staff increased to 15, and three endoscopy engineers are working with us.
The Gastrointestinal Endoscopy Division has 13 staff physicians in the National Cancer Center Hospital (NCCH), and in the Division of Screening Technology of the Center for Public Health Sciences, four chief residents, nine residents, one trainee, and several rotating residents.
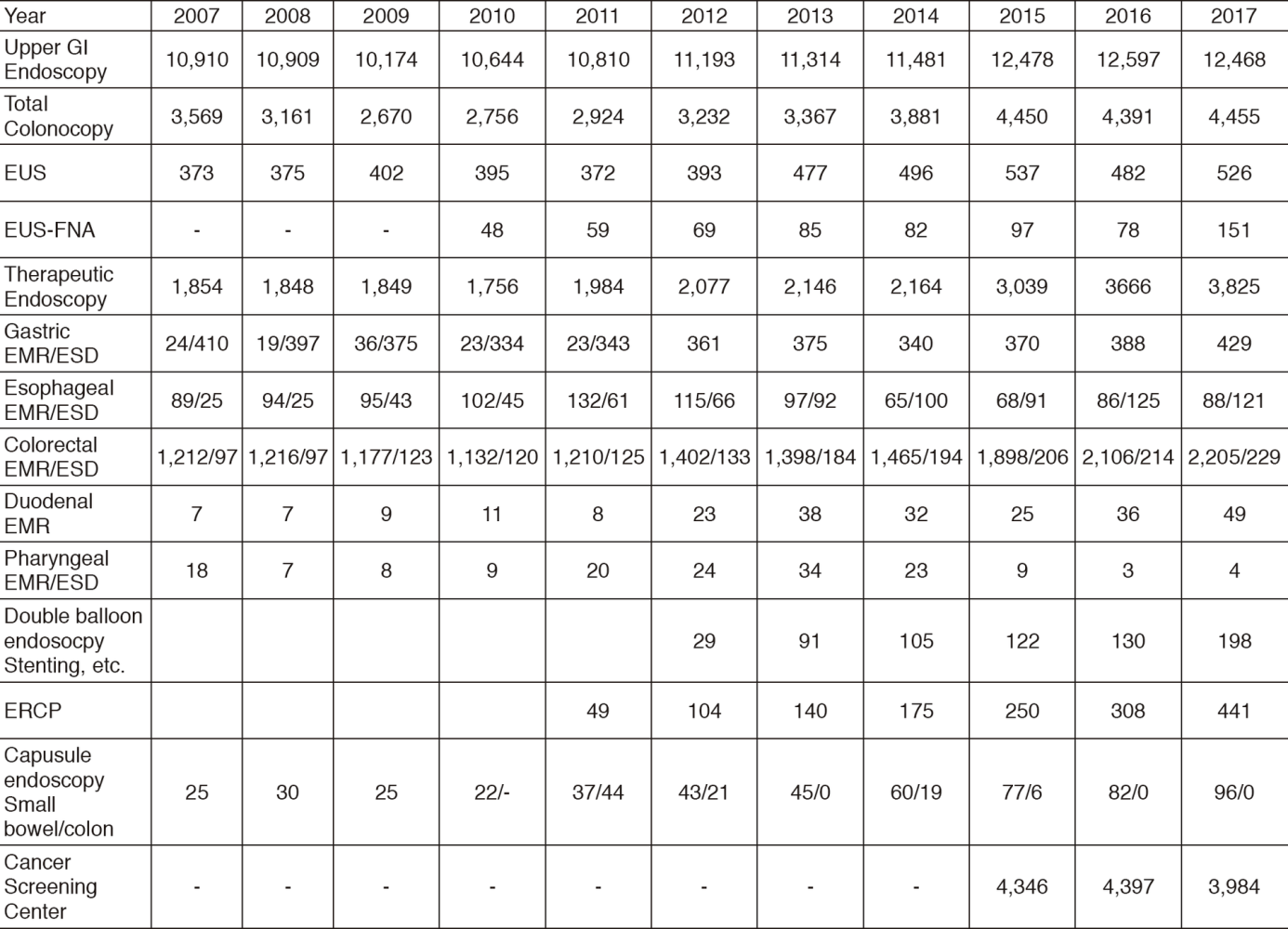
Table 1. Chronological Trend of Total number of Diagnostic and Therapeutic Gastrointestinal Endoscopic Procedures
The Respiratory Endoscopy Division has three staff members, and the total number of bronchoscopies and therapeutic procedures has been dramatically increased.
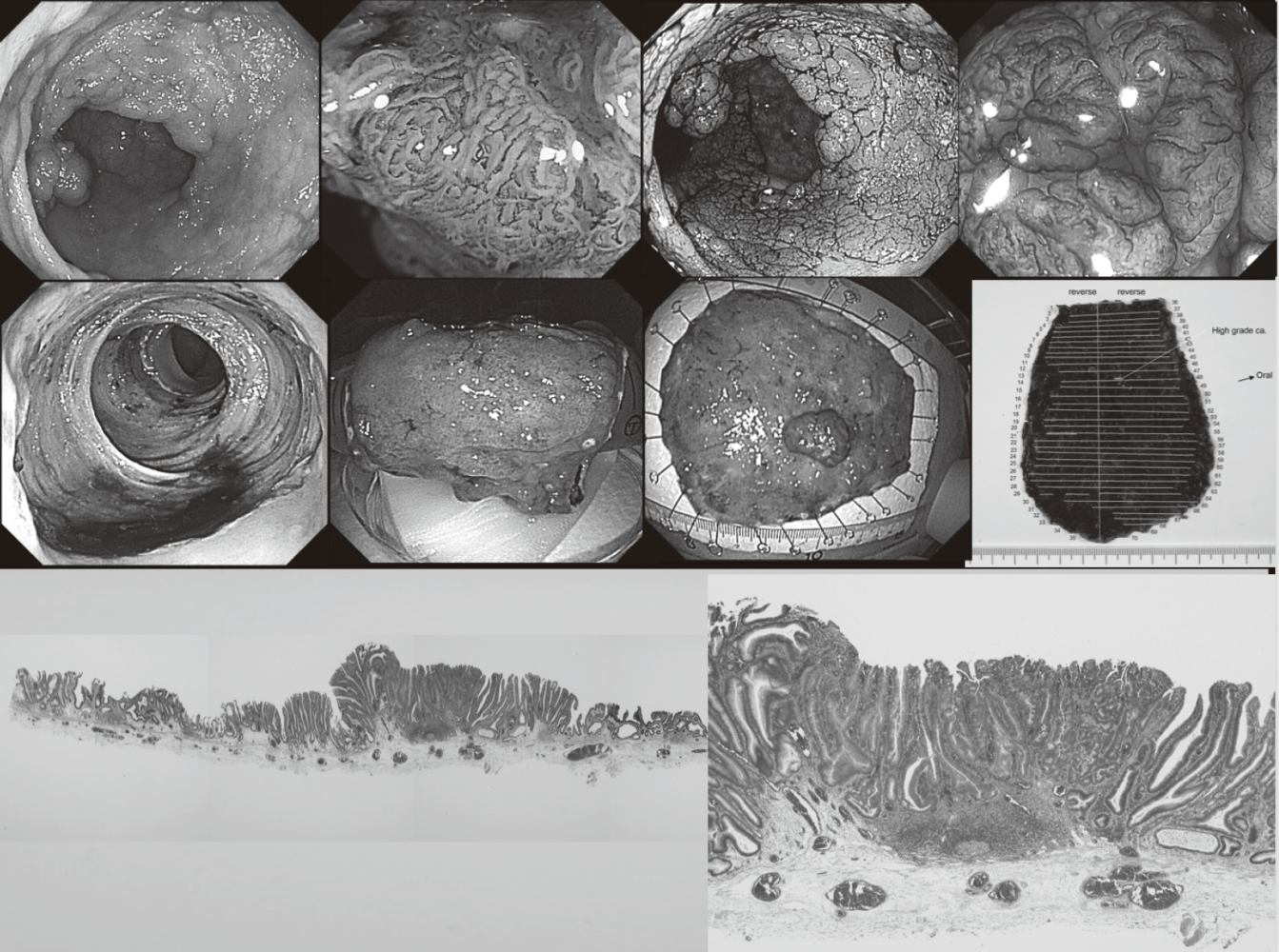
Dramatic developments have recently changed the operational mechanism and design of endoscopes along with a variety of accessory devices and instruments, so clinical applications using the latest equipment are evolving on a continuous basis. In the Gastrointestinal Endoscopy Division, more advanced and technically difficult endoscopic treatments such as endoscopic submucosal dissection (ESD) are being used in place of conventional endoscopic mucosal resection (EMR) not only for early gastric cancer, but also for superficial esophageal and colorectal neoplasms. In addition, educational activities are an important part of our division's activities with many Japanese medical students, residents and staff physicians as well as approximately 130 overseas post-graduate physicians attending our training courses annually.
Our Endoscopy Center was authorized as one of WEO Centers of Excellence by the World Endoscopy Organization (WEO) and got an award during Gastro 2017 in Hyderabad. This is an honorable award for us because there are only 17 famous international centers in the world and just two centers in Japan.
Routine Activities in Gastrointestinal (GI) Endoscopy
Various diagnostic techniques including chromoendoscopy, magnifying endoscopy, and endoscopic ultrasonography (EUS) are used to detect and evaluate early malignant lesions. Capsule endoscopy has also been accepted as being far less invasive. In our facility, small intestine capsule endoscopy has been performed since 2005. In order to obtain a more accurate endoscopic diagnosis of gastrointestinal disease, we routinely use the recently developed narrow-band imaging (NBI) system and blue laser imaging (BLI) system. A total of 12,468, 4,455, 526, 151, 441, 96, and 198 screening and/or diagnostic procedures by gastroscopy, colonoscopy, EUS, EUS-fine needle aspiration (EUS-FNA), endoscopic retrograde cholangiopancreatography (ERCP), capsule endoscopy and double balloon endoscopies, respectively, were performed in 2017 (Table 1).
Due to the increasing number of patients with superficial gastrointestinal neoplasms, the number of therapeutic endoscopy procedures is also increasing in this field. In 2017, 3,125 endoscopic resections were carried out (pharynx four, esophagus 209, stomach 429, duodenum 49 and colon 2,434). Among these, ESD, which was developed for large en-bloc resections with a low-risk of local recurrence, was performed for 121 superficial esophageal cancers, 429 early gastric cancers and 229 superficial colorectal neoplasms. For colorectal ESDs and some esophageal ESDs, the newly developed ball-tip bipolar needle knife (Jet B-knife) and IT-knife nano were used together with CO2 insufflation. Our colleagues originally developed these procedures and devices.
ESD achieves a higher en-bloc resection rate compared to the standard EMR technique and is less invasive than a surgical operation while EUS-FNA provides a less invasive procedure to improve diagnosis for patients with pancreatic tumors, lymph-node swelling, submucosal tumors of the GI tract, etc.
Image-reading conferences are held regularly and we attend all clinical conferences in the Surgery, Oncology, Radiology and Pathology Divisions to discuss and decide on treatment strategies.
Clinical Activities in GI Endoscopy
Our efforts have been focused on new diagnostic and therapeutic strategies. For more accurate endoscopic diagnosis of gastrointestinal disease, we are utilizing the NBI and BLI systems that enable us to narrow the spectral transmittance bandwidth of the optical filters used in the light source of electronic endoscope systems. In addition, we have introduced an endocytoscopy system. This system can magnify lesions up to 500x magnification and visualize nuclear atypia.
Clinical Trials in GI Endoscopy
We have organized several multicenter study groups to evaluate the efficacy and clinical impact of newly developed endoscopies and medical devices prospectively.
Esophagus
We are currently enrolling our patients in several multicenter randomized controlled trials (RCTs).
First, a phase II/III study has been introduced to compare endoscopic balloon dilatation combined with steroid to radial incision and cutting combined with steroid for refractory anastomotic stricture after esophagectomy (JCOG1207: RICS study).
Second, a phase III study is ongoing to compare oral steroid administration to local steroid injection therapy for the prevention of esophageal stricture after endoscopic submucosal dissection (JCOG1217: Steroid EESD P3).
In collaboration with TWins (Tokyo Women's Medical University ‐ Waseda University Joint Institution for Advanced Biomedical Sciences), we have conducted a clinical trial of cell sheet-based regenerative medicine, which could reduce complications such as severe stenosis and perforation related to intensive balloon dilations. This cell sheet-based regenerative medicine is one of innovation in the gastrointestinal field and we believe that cell-based regenerative medicine would be useful to improve quality of life of patients after esophageal ESD.
Endoscopic resection of esophageal cancer was widely spread and the several innovations were developed to prevent post-ESD esophageal stricture as mentioned above. However, optimal additional treatment strategy of endoscopic resection for patients with T1a-MM and T1b-SM1 esophageal cancer, particularly esophageal adenocarcinoma is still under discussion and further prospective studies are warranted. A multicenter prospective observational cohort study is ongoing to investigate long-term outcomes of those patients.
An RCT comparing conventional ESD versus ESD with counter-traction for superficial esophageal cancer (CONNECT-E trial) is now ongoing at seven institutions in Japan since January 2017. The usefulness of the traction method using clip with line technique in gastric ESD has been proven in the multicenter RCT at our same group in 2017, and we try to make the clear evidence in esophageal ESD as well as in gastric ESD.
A non-randomized study for the usefulness of endoscopic ultrasonography is ongoing to compare with magnified endoscopy with narrow band imaging for diagnosing cancer invasion depth of clinical stage IA esophageal squamous cell carcinoma (JCOG1604: Odyssey trial).
Stomach
A nationwide cancer registry system has been developed for early gastric cancer treated with EMR/ESD. A five-year multicenter prospective cohort study has been ongoing using this cancer registry system since 2010 (J-WEB/EGC).
In addition, we have completed two multicenter RCTs. First one is a CONNECT-G trial to investigate the usefulness of endo-clip connecting dental floss (DFC) during gastric ESD that has a potential efficacy making a better view by traction with DFC. Second one is an RCT to compare the second-generation NBI with white-light imaging (WLI) for detection of early gastric cancer (EGC Detection Trial).
Duodenum
A non-randomized confirmatory trial of cold snare polypectomy for superficial non-ampullary duodenal epithelial tumor (D-COP trial) is now ongoing at more than 100 institutions in Japan since 2017. Recently, cold snare polypectomy is widely used in the colorectal region and it is expected that same concept can be applied for duodenal small tumor (familial adenomatous polyposis [FAP] is excluded from this trial).
Pancreas
We prospectively evaluated the efficacy and safety of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) for pancreatic solid lesions in multicenters in Japan. This study was designed as a prospective cohort study conducted at the following five hospitals in Japan: The NCCH, Tokyo Medical University, Aichi Cancer Center Hospital, Gifu University Hospital, and Fukushima Medical University Aizu Medical Center. Two hundred and forty-nine patients were enrolled from November 2011 to June 2013. Diagnostic sensitivity of EUS-FNA in this study was 97.2%. Diagnostic specificity, accuracy, positive predictive value, and negative predictive value were 88.0%, 96.2%, 100%, 81.4%, respectively. Complication after seven days was 1.6%. We could confirm the efficacy and safety of EUS-FNA for pancreatic solid lesions is quite satisfied.
Colorectum
RCTs concerning colorectal neoplasms are ongoing as well.
The Japan Polyp Study (JPS), a multicenter RCT conducted at 11 participating centers was initiated in 2003. The aim of this study was to assess whether follow-up colonoscopy using high-definition colonoscope at three years as well as at both one and three years would detect important lesions including non-polypoid colorectal neoplasia. The JPS will provide preexisting comorbidity data, including the prevalence of both flat and depressed colorectal lesions, the quality of colonoscopy, and the risk of colorectal cancer (CRC). Furthermore, the study will clarify the long-term impact of colonoscopic removal on mortality due to CRC. The evidence will enable to elaborate the fundamental basis for the updated Japanese surveillance guidelines (Participants of JPS: 3,926, JPS Cohort: 1,290).
Little is known about the long-term outcomes of patients with submucosal invasive CRC who undergo endoscopic or surgical resection. We performed a retrospective analysis of long-term outcomes of patients treated for submucosal colon and rectal cancer. We collected data from 549 patients with submucosal colon cancer and 209 with submucosal rectal cancer who underwent endoscopic or surgical resection at six institutions, over a median follow-up period of 60.5 months. We assessed recurrence rates, five-year disease-free survival, and five-year overall survival. As a result of patients treated with only endoscopic resection, the risk for local recurrence was significantly higher in high-risk patients with submucosal rectal cancer than patients with submucosal colon cancer. The addition of surgery is therefore recommended for patients with submucosal rectal cancer with pathology features indicating a high risk of tumor progression (Gastroenterology 2012). Considering this study result, we have completed a prospective cohort study for the possibility of chemo-radiotherapy (CRT) for high-risk rectal submucosal cancer after endoscopic resections. We are playing a leading part to conduct a multicenter single-arm study (JCOG1612) for the possibility of CRT for high-risk rectal submucosal cancer after endoscopic resections. When this study result shows a non-
inferiority of CRT compared to surgery, we could propose a new non-invasive treatment strategy for rectal T1 cancer patients.
A nationwide cancer registry system has also been developed for early CRC treated with ESD. A five-year multicenter prospective cohort study has been ongoing using this cancer registry system since 2013. A total of 2,066 patients was enrolled to this multicenter cohort study and this should be the largest cohort study in colorectal ESD in the world.
A multicenter RCT to compare the detectability of colorectal neoplastic lesions using a novel endoscopic system with blue laser imaging (BLI) was completed. A newly developed system that uses BLI improves the detection of adenomatous lesions compared with WLI (Clinical trial registration number: UMIN 000014555) and published in Gastrointest Endosc. 2017 Jan 29.
The other multicenter RCT to compare the adenoma miss rate between new full-spectrum endoscopy (Fuse) and conventional colonoscopy was completed. This study revealed a significant lower adenoma miss rate and higher ADR in Fuse group and the result has been published in Gastrointestinal Endoscopy.
A multicenter RCT to clarify the efficacy of autofluorescence imaging (AFI) on flat adenoma detection has been completed (A-FLAT trial).
We have just started an Endoscopy Tissue Bank (ETB) first in the world and will collaborate with the University of Tokyo and the Jikei University School of Medicine for this big project. This ETB will be extended to all Cancer Hospitals in the future.
We have conducted a multicenter prospective cohort study on colorectal neuroendocrine tumors (NETs) since January 2017. This study is expected to provide new important findings on colorectal NETs.
A multicenter prospective cohort study on T1 CRC has also been performed since May 2017. This study is collecting many T1 CRC cases from over 70 institutions all over Japan and will bring important information on the management of T1 cancer.
J-CAPP Study II
To evaluate the influence of low-dose, enteric-
coated aspirin tablets (100 mg/day for four years) on colorectal tumor recurrence, we have conducted a multicenter prospective study since 2015 (Chief conductor: Hideki Ishikawa, M.D, Kyoto Prefectural University of Medicine). At the moment, a total of 3,584 patients was enrolled in this study.
Molecular and fluorescence Imaging and Database Study
Molecular imaging endoscopy is one of a new era for very early cancer diagnosis and detection of metastasis. We have started a collaborative study with the Departments of Endoscopy, Colorectal Surgery, Gastric Surgery, and Pathology and Clinical Laboratories, the NCC, Research Institute, the University of Tokyo, and the Jikei University School of Medicine.
Probe-based confocal laser endomicroscopy (pCLE) allows real-time, in vivo high resolution imaging of the gastrointestinal epithelium at a cellular level. We are going to conduct a multicenter prospective study using an advanced medical treatment system (type B) supported by the Japan Agency for Medical Research and Development (AMED) to evaluate the diagnostic yield of pCLE for gastric neoplasms.
We have been collaborating with the Japan Gastroenterological Endoscopy Society (JGES) in order to build a Japan endoscopy database (JED) of gastrointestinal endoscopies including not only therapeutic but also diagnostic procedures. This all Japan project is named JED and has the potential to construct the largest and most precise database of all endoscopic procedures. Japanese endoscopists are well known as most excellent endoscopists, therefore, we can create lots of evidences using this huge endoscopy database from now.
Research and development of new endoscopy using artificial intelligence (AI)
Recent development of artificial intelligence (AI) using deep learning is expected to apply in precision medicine. We have been researching and developing new endoscopic systems using AI. First, in order to support endoscopist's detection of CRC and precancerous lesions during colonoscopy by AI, we have been researching and developing a software program using convolutional neural networks based on mathematical morphology and hardware, which works in real-time. We will extend this system to genomic data and other gastrointestinal organs, such as the stomach and esophagus, in the future.
Second, we started a multicenter image analyzing study to compare a new automatic diagnosis system using AI with endoscopist's diagnosis of colorectal lesions using endocytoscopy.
Research and development of new endoscopy
Olympus Medical Systems Corp. has opened a laboratory at our new research center and we are collaborating with them for developing innovative endoscopy systems and devices.
List of papers published in January 2017 - March 2018
Journal
1. Nakamura F, Saito Y, Haruyama S, Sekiguchi M, Yamada M, Sakamoto T, Nakajima T, Yamamoto S, Murakami Y, Ishikawa H, Matsuda T. Short-term Prospective Questionnaire Study of Early Postoperative Quality of Life After Colorectal Endoscopic Submucosal Dissection. Dig Dis Sci, 62:3325-3335, 2017
2. Saito Y, Bhatt A, Matsuda T. Colorectal endoscopic submucosal dissection and its journey to the West. Gastrointest Endosc, 86:90-92, 2017
3. Nakanishi H, Doyama H, Ishikawa H, Uedo N, Gotoda T, Kato M, Nagao S, Nagami Y, Aoyagi H, Imagawa A, Kodaira J, Mitsui S, Kobayashi N, Muto M, Takatori H, Abe T, Tsujii M, Watari J, Ishiyama S, Oda I, Ono H, Kaneko K, Yokoi C, Ueo T, Uchita K, Matsumoto K, Kanesaka T, Morita Y, Katsuki S, Nishikawa J, Inamura K, Kinjo T, Yamamoto K, Yoshimura D, Araki H, Kashida H, Hosokawa A, Mori H, Yamashita H, Motohashi O, Kobayashi K, Hirayama M, Kobayashi H, Endo M, Yamano H, Murakami K, Koike T, Hirasawa K, Miyaoka Y, Hamamoto H, Hikichi T, Hanabata N, Shimoda R, Hori S, Sato T, Kodashima S, Okada H, Mannami T, Yamamoto S, Niwa Y, Yashima K, Tanabe S, Satoh H, Sasaki F, Yamazato T, Ikeda Y, Nishisaki H, Nakagawa M, Matsuda A, Tamura F, Nishiyama H, Arita K, Kawasaki K, Hoppo K, Oka M, Ishihara S, Mukasa M, Minamino H, Yao K. Evaluation of an e-learning system for diagnosis of gastric lesions using magnifying narrow-band imaging: a multicenter randomized controlled study. Endoscopy, 49:957-967, 2017
4. Ngamruengphong S, Abe S, Oda I. Endoscopic Management of Early Gastric Adenocarcinoma and Preinvasive Gastric Lesions. Surg Clin North Am, 97:371-385, 2017
5. Tanabe S, Ishido K, Matsumoto T, Kosaka T, Oda I, Suzuki H, Fujisaki J, Ono H, Kawata N, Oyama T, Takahashi A, Doyama H, Kobayashi M, Uedo N, Hamada K, Toyonaga T, Kawara F, Tanaka S, Yoshifuku Y. Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: a multicenter collaborative study. Gastric cancer, 20:45-52, 2017
6. Abe S, Iyer PG, Oda I, Kanai N, Saito Y. Approaches for stricture prevention after esophageal endoscopic resection. Gastrointest Endosc, 86:779-791, 2017
7. Saito Y, Sumiyama K, Chiu PW. Robot assisted tumor resection devices. Expert Rev Med Devices, 14:657-662, 2017
8. Purchiaroni F, Nakajima T, Sakamoto T, Abe S, Saito Y. Over-The-Scope-Clip pre-mounted onto a double balloon enteroscope for fast and successful closure of post-EMR jejunal perforation: case report. BMC Gastroenterol, 17:152, 2017
9. Shichijo S, Uedo N, Saito Y. Report of the international symposiums at the 93rd Congress of Japan Gastroenterological Endoscopy Society in Osaka, 2017. Dig Endosc, 29:761-764, 2017
10. Yokoyama A, Katada C, Yokoyama T, Yano T, Kaneko K, Oda I, Shimizu Y, Doyama H, Koike T, Takizawa K, Hirao M, Okada H, Yoshii T, Konishi K, Yamanouchi T, Tsuda T, Omori T, Kobayashi N, Suzuki H, Tanabe S, Hori K, Nakayama N, Kawakubo H, Ishikawa H, Muto M. Alcohol abstinence and risk assessment for second esophageal cancer in Japanese men after mucosectomy for early esophageal cancer. PLoS One, 12:e0175182, 2017
11. Tamai N, Saito Y, Sakamoto T, Nakajima T, Matsuda T, Sumiyama K, Tajiri H, Koyama R, Kido S. Effectiveness of computer-aided diagnosis of colorectal lesions using novel software for magnifying narrow-band imaging: a pilot study. Endosc Int Open, 5:E690-E694, 2017
12. Sekiguchi M, Oda I. High miss rate for gastric superficial cancers at endoscopy: what is necessary for gastric cancer screening and surveillance using endoscopy? Endoscopy international open, 5:E727-E728, 2017
13. Sekiguchi M, Oda I, Suzuki H, Abe S, Nonaka S, Yoshinaga S, Taniguchi H, Sekine S, Saito Y. Clinical outcomes and prognostic factors in gastric cancer patients aged >/=85 years undergoing endoscopic submucosal dissection. Gastrointest Endosc, 85:963-972, 2017
14. Yamada M, Saito Y, Takamaru H, Sasaki H, Yokota T, Matsuyama Y, Sato Y, Sakamoto T, Nakajima T, Taniguchi H, Sekine S, Matsuda T. Long-term clinical outcomes of endoscopic submucosal dissection for colorectal neoplasms in 423 cases: a retrospective study. Endoscopy, 49:233-242, 2017
15. Hotta K, Matsuda T, Kakugawa Y, Ikematsu H, Kobayashi N, Kushima R, Hozawa A, Nakajima T, Sakamoto T, Mori M, Fujii T, Saito Y. Regional colorectal cancer screening program using colonoscopy on an island: a prospective Nii-jima study. Jpn J Clin Oncol, 47:118-122, 2017
16. Suzuki H, Oda I, Abe S, Sekiguchi M, Nonaka S, Yoshinaga S, Saito Y, Fukagawa T, Katai H. Clinical outcomes of early gastric cancer patients after noncurative endoscopic submucosal dissection in a large consecutive patient series. Gastric Cancer, 20:679-689, 2017
17. Nakamura K, Nonaka S, Nakajima T, Yachida T, Abe S, Sakamoto T, Suzuki H, Yoshinaga S, Oda I, Matsuda T, Sekine S, Kanemitsu Y, Katai H, Saito Y, Hirota S. Clinical outcomes of gastric polyps and neoplasms in patients with familial adenomatous polyposis. Endosc Int Open, 5:E137-E145, 2017
18. Ikematsu H, Sakamoto T, Togashi K, Yoshida N, Hisabe T, Kiriyama S, Matsuda K, Hayashi Y, Matsuda T, Osera S, Kaneko K, Utano K, Naito Y, Ishihara H, Kato M, Yoshimura K, Ishikawa H, Yamamoto H, Saito Y. Detectability of colorectal neoplastic lesions using a novel endoscopic system with blue laser imaging: a multicenter randomized controlled trial. Gastrointest Endosc, 86:386-394, 2017
19. Ishihara R, Oyama T, Abe S, Takahashi H, Ono H, Fujisaki J, Kaise M, Goda K, Kawada K, Koike T, Takeuchi M, Matsuda R, Hirasawa D, Yamada M, Kodaira J, Tanaka M, Omae M, Matsui A, Kanesaka T, Takahashi A, Hirooka S, Saito M, Tsuji Y, Maeda Y, Yamashita H, Oda I, Tomita Y, Matsunaga T, Terai S, Ozawa S, Kawano T, Seto Y. Risk of metastasis in adenocarcinoma of the esophagus: a multicenter retrospective study in a Japanese population. J Gastroenterol, 52:800-808, 2017
20. Mejia-Perez LK, Abe S, Stevens T, Parsi MA, Jang SN, Oda I, Vargo JJ, Saito Y, Bhatt A. A minimally invasive treatment for early GI cancers. Cleve Clin J Med, 84:707-717, 2017
21. Federico Iacopini, Takuji Gotoda,Fabrizio Montagnese, Fabio Andrei, Yutaka Saito. Underwater endoscopic submucosal dissection of a nonpolypoid super?cial tumor spreading into the appendix. VideoGIE, 2:82-84, 2017
22. Abe S, Oda I, Suzuki H, Yoshinaga S, Saito Y. Insulated tip knife tunneling technique with clip line traction for safe endoscopic submucosal dissection of large circumferential esophageal cancer. VIDEOGIE, 2:342-345, 2017
23. Yano T, Yoda Y, Nomura S, Toyosaki K, Hasegawa H, Ono H, Tanaka M, Morimoto H, Horimatsu T, Nonaka S, Kaneko K, Sato A. Prospective trial of biodegradable stents for refractory benign esophageal strictures after curative treatment of esophageal cancer. Gastrointest Endosc, 86:492-499, 2017
24. Maeda M, Nakajima T, Oda I, Shimazu T, Yamamichi N, Maekita T, Asada K, Yokoi C, Ando T, Yoshida T, Nanjo S, Fujishiro M, Gotoda T, Ichinose M, Ushijima T. High impact of methylation accumulation on metachronous gastric cancer: 5-year follow-up of a multicentre prospective cohort study. Gut, 66:1721-1723, 2017
25. Abe S, Minagawa T, Tanaka H, Oda I, Saito Y. Successful endoscopic closure using over-the-scope clip for delayed stomach perforation caused by nasogastric tube after endoscopic submucosal dissection. Endoscopy, 49:E56-E57, 2017
26. Iacopini F, Saito Y, Bella A, Gotoda T, Rigato P, Elisei W, Montagnese F, Iacopini G, Costamagna G. Colorectal endoscopic submucosal dissection: predictors and neoplasm-related gradients of difficulty. Endosc Int Open, 5:E839-E846, 2017
27. Yamada M, Oda I, Tanaka H, Abe S, Nonaka S, Suzuki H, Yoshinaga S, Kuchiba A, Koyanagi K, Igaki H, Taniguchi H, Sekine S, Saito Y, Tachimori Y. Tumor location is a risk factor for lymph node metastasis in superficial Barrett's adenocarcinoma. Endoscopy international open, 5:E868-E874, 2017
28. Mortagy M, Mehta N, Parsi MA, Abe S, Stevens T, Vargo JJ, Saito Y, Bhatt A. Magnetic anchor guidance for endoscopic submucosal dissection and other endoscopic procedures. World J Gastroenterol, 23:2883-2890, 2017
29. Spychalski M, Skulimowski A, Dziki A, Saito Y. Colorectal endoscopic submucosal dissection (ESD) in the West - when can satisfactory results be obtained? A single-operator learning curve analysis. Scand J Gastroenterol, 52:1442-1452, 2017
30. Nishiumi S, Kobayashi T, Kawana S, Unno Y, Sakai T, Okamoto K, Yamada Y, Sudo K, Yamaji T, Saito Y, Kanemitsu Y, Okita NT, Saito H, Tsugane S, Azuma T, Ojima N, Yoshida M. Investigations in the possibility of early detection of colorectal cancer by gas chromatography/triple-quadrupole mass spectrometry. Oncotarget, 8:17115-17126, 2017
31. Tanabe S, Hirabayashi S, Oda I, Ono H, Nashimoto A, Isobe Y, Miyashiro I, Tsujitani S, Seto Y, Fukagawa T, Nunobe S, Furukawa H, Kodera Y, Kaminishi M, Katai H. Gastric cancer treated by endoscopic submucosal dissection or endoscopic mucosal resection in Japan from 2004 through 2006: JGCA nationwide registry conducted in 2013. Gastric cancer, 20:834-842, 2017
32. Kanesaka T, Uedo N, Yao K, Ezoe Y, Doyama H, Oda I, Kaneko K, Kawahara Y, Yokoi C, Sugiura Y, Ishikawa H, Takeuchi Y, Arao M, Iwatsubo T, Iwagami H, Matsuno K, Muto M, Saito Y, Tomita Y. Multiple convex demarcation line for prediction of benign depressed gastric lesions in magnifying narrow-band imaging. Endosc Int Open, 6:E145-E155, 2018
33. Hasuike N, Ono H, Boku N, Mizusawa J, Takizawa K, Fukuda H, Oda I, Doyama H, Kaneko K, Hori S, Iishi H, Kurokawa Y, Muto M. A non-randomized confirmatory trial of an expanded indication for endoscopic submucosal dissection for intestinal-type gastric cancer (cT1a): the Japan Clinical Oncology Group study (JCOG0607). Gastric Cancer, 21:114-123, 2018
34. Morita S, Arai Y, Sugawara S, Sone M, Sakamoto Y, Okusaka T, Yoshinaga S, Saito Y, Terai S. Antireflux Metal Stent for Initial Treatment of Malignant Distal Biliary Obstruction. Gastroenterol Res Pract, 2018:3805173, 2018
35. Watanabe T, Muro K, Ajioka Y, Hashiguchi Y, Ito Y, Saito Y, Hamaguchi T, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kawano H, Kinugasa Y, Kokudo N, Murofushi K, Nakajima T, Oka S, Sakai Y, Tsuji A, Uehara K, Ueno H, Yamazaki K, Yoshida M, Yoshino T, Boku N, Fujimori T, Itabashi M, Koinuma N, Morita T, Nishimura G, Sakata Y, Shimada Y, Takahashi K, Tanaka S, Tsuruta O, Yamaguchi T, Yamaguchi N, Tanaka T, Kotake K, Sugihara K. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol, 23:1-34, 2018
36. Katai H, Ishikawa T, Akazawa K, Isobe Y, Miyashiro I, Oda I, Tsujitani S, Ono H, Tanabe S, Fukagawa T, Nunobe S, Kakeji Y, Nashimoto A. Five-year survival analysis of surgically resected gastric cancer cases in Japan: a retrospective analysis of more than 100,000 patients from the nationwide registry of the Japanese Gastric Cancer Association (2001-2007). Gastric Cancer, 21:144-154, 2018
37. Hideyuki Ishida, Tatsuro Yamaguchi, Kohji Tanakaya, Kiwamu Akagi, Yasuhiro Inoue, Kensuke Kumamoto, Hideki Shimodaira, Shigeki Sekine, Toshiaki Tanaka, Akiko Chino, Naohiro Tomita, Takeshi Nakajima, Hirotoshi Hasegawa, Takao Hinoi, Akira Hirasawa, Yasuyuki Miyakura, Yoshie Murakami, Kei Muro, Yoichi Ajioka, Yojiro Hashiguchi, Yoshinori Ito, Yutaka Saito, Tetsuya Hamaguchi, Megumi Ishiguro, Soichiro Ishihara, Yukihide Kanemitsu, Hiroshi Kawano, Yusuke Kinugasa, Norihiro Kokudo, Keiko Murofushi, Takako Nakajima, Shiro Oka, Yoshiharu Sakai, Akihiko Tsuji, Keisuke Uehara, Hideki Ueno, Kentaro Yamazaki, Masahiro Yoshida, Takayuki Yoshino, Narikazu Boku, Takahiro Fujimori, Michio Itabashi, Nobuo Koinuma, Takayuki Morita, Genichi Nishimura, Yuh Sakata, Yasuhiro Shimada, Keiichi Takahashi, Shinji Tanaka, Osamu Tsuruta, Toshiharu Yamaguchi, Kenichi Sugihara, Toshiaki Watanabe, Japanese Society for Cancer of the Colon and Rectum.Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2016 for the Clinical Practice of Hereditary Colorectal Cancer (Translated Version). J Anus Rectum Colon, 2:S1-S51, 2018
38. Kodashima S, Tanaka K, Matsuda K, Fujishiro M, Saito Y, Ohtsuka K, Oda I, Katada C, Kato M, Kida M, Kobayashi K, Hoteya S, Horimatsu T, Matsuda T, Muto M, Yamamoto H, Ryozawa S, Iwakiri R, Kutsumi H, Miyata H, Kato M, Haruma K, Fujimoto K, Uemura N, Kaminishi M, Tajiri H. First progress report on the Japan Endoscopy Database project. Dig Endosc, 30:20-28, 2018
39. Matsuda K, Tanaka K, Fujishiro M, Saito Y, Ohtsuka K, Oda I, Katada C, Kato M, Kida M, Kobayashi K, Hoteya S, Horimatsu T, Kodashima S, Matsuda T, Muto M, Yamamoto H, Ryozawa S, Iwakiri R, Kutsumi H, Miyata H, Kato M, Haruma K, Fujimoto K, Uemura N, Kaminishi M, Tajiri H. Design paper: Japan Endoscopy Database (JED): A prospective, large database project related to gastroenterological endoscopy in Japan. Dig Endosc, 30:5-19, 2018
40. Yamashita S, Kishino T, Takahashi T, Shimazu T, Charvat H, Kakugawa Y, Nakajima T, Lee YC, Iida N, Maeda M, Hattori N, Takeshima H, Nagano R, Oda I, Tsugane S, Wu MS, Ushijima T. Genetic and epigenetic alterations in normal tissues have differential impacts on cancer risk among tissues. Proc Natl Acad Sci U S A, 115:1328-1333, 2018
Book
1. Iacopini F, Saito Y. Colorectal Endoscopic Submucosal Dissection. In: Facciorusso, Antonio, Muscatiello, Nicola (eds), Colon Polypectomy, Springer International Publishing AG, pp 73-88, 2018