Annual Report 2017
Department of Hepatobiliary and Pancreatic Surgery
Kazuaki Shimada, Minoru Esaki, Yoji Kishi, Satoshi Nara, Keiichi Akahoshi
Introduction
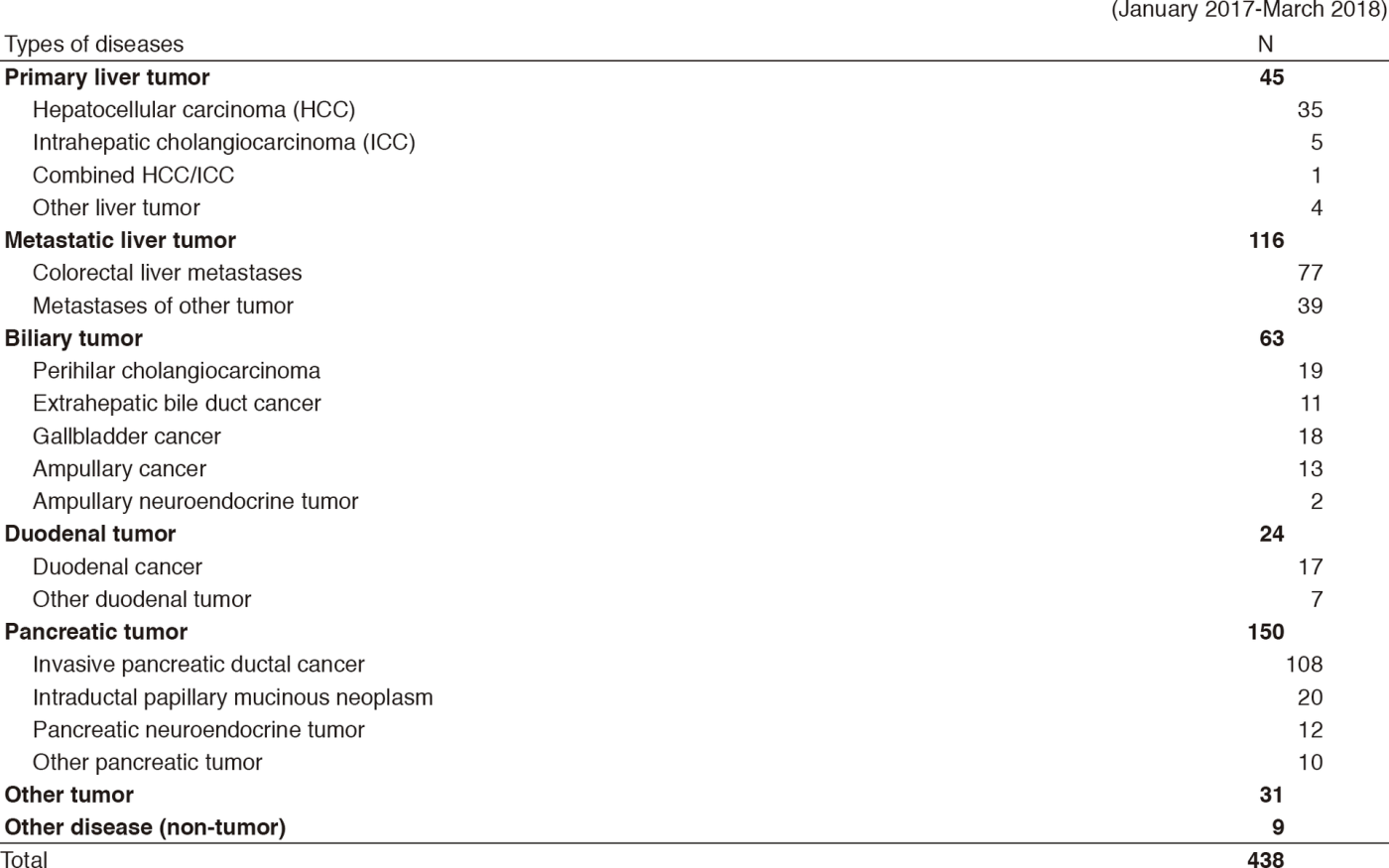
The Department of Hepatobiliary and Pancreatic (HBP) Surgery deals with malignant neoplasms arising from the liver, biliary tract including the gallbladder, and pancreas. We conduct aggressive surgical treatment and multidisciplinary treatment in cooperation with the Department of Diagnostic Radiology, the Department of Hepatobiliary and Pancreatic (HBP) Oncology, and the Pathology Division.
Our team and what we do
Our department consists of four staff surgeons and we perform more than 300 surgeries each year, along with one chief resident and three or four residents. Occasionally, trainees from home and abroad join our group.
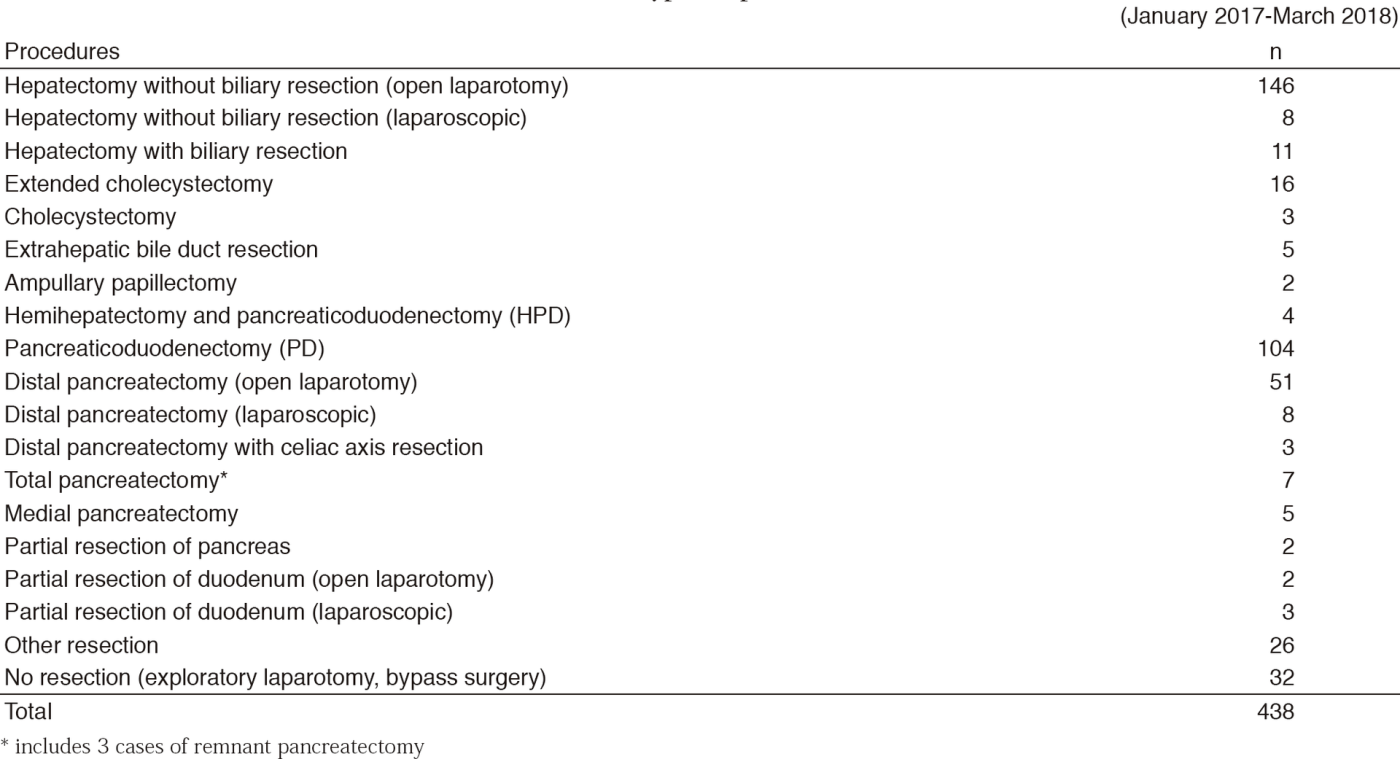
1. Operation and perioperative care
One staff surgeon and one resident are in charge of each patient, and conduct an operation and provide postoperative care. The chief resident attends all the operations, supervises residents and manages the care of all inpatients.
2. Conferences
We hold several clinical or educational conferences on the treatment of HBP malignancies. At the "Ward Conference", clinical conditions of the perioperative patients and surgical strategies for preoperative cases are discussed. At the "Cherry Conference", surgeons and radiologists discuss imaging studies of patients scheduled for surgery. The "HBP Case Conference" is held by surgeons and medical oncologists to discuss treatment strategies. The "Micro Conference" is a pathological conference on postoperative cases, where surgeons, radiologists, and pathologists participate in the discussion.
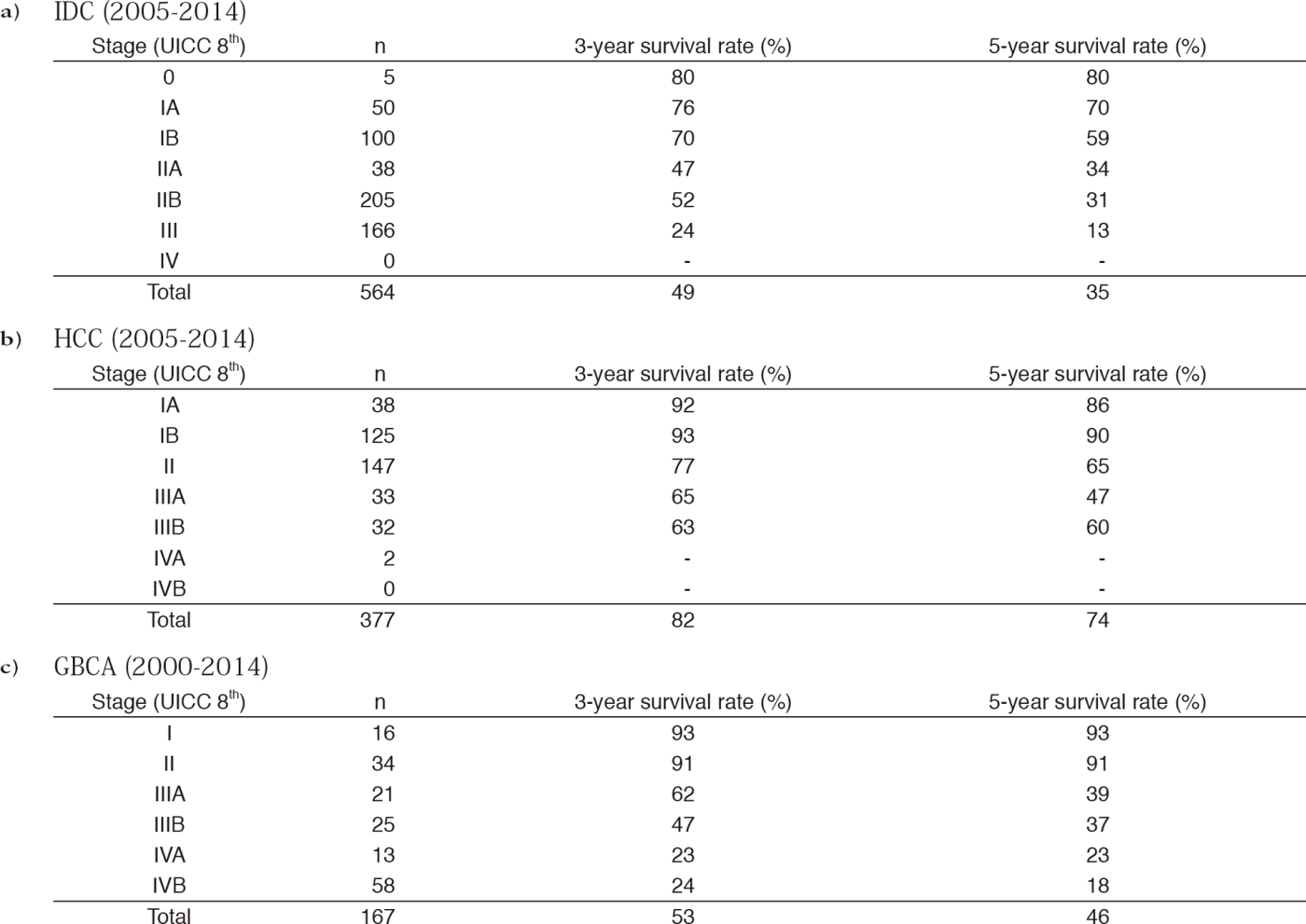
3. Surgical strategies for HBP malignancies
Hepatocellular carcinoma (HCC): Surgical resection is usually indicated in patients with solitary or only a few tumors, and with favorable hepatic function. A huge tumor or HCC with macroscopic vasculobiliary tumor thrombosis is also indicated for resection as long as sufficient hepatic function and remnant liver volume is expected. Alternative treatments other than hepatectomy are performed in cooperation with medical oncologists and radiologists.
Pancreatic cancer: Multidisciplinary treatment with curative resection followed by adjuvant chemotherapy is the standard strategy. According to the recent advancement of systemic chemotherapy with improved response, the opportunity of surgical resection for initially unresectable cancer due to locally extensive disease has been increasing.
Biliary cancer ‐ cholangiocarcinoma and gallbladder cancer: On the basis of careful imaging evaluation of cancer extension, a wide variety of surgical resections can be applied to biliary cancer. Major resection including pancreatoduodenectomy or extended hemihepatectomy with extrahepatic bile duct resection with or without vascular reconstruction is frequently indicated. Safe and curative resection with careful perioperative management is mandatory.
Laparoscopic surgery: For liver tumors located in the peripheral site, laparoscopic lateral bisegmentectomy or partial resection is considered as a choice of treatment. Laparoscopic distal pancreatectomy is indicated for low-grade
malignant tumors.
Research activities
Dr. Shimada et al. conducts two multiinstitutional randomized trials. One is to evaluate the safety of drain tube free hepatectomy (ND-trial), in which the patient registration and data analyses have finished. The other is to evaluate the efficacy of administrating digestive enzymes to prevent postoperative hepatic steatosis in patients who underwent pancreaticoduodenectomy (ESOP Trial), in which patient recruitment is on-going.
Dr. Kishi attends an international collaboration project by EORTC (European Organisation for Research and Treatment of Cancer) and JCOG (Japan Clinical Oncology Group) as a Japanese side manager. The project is to evaluate the accuracy of Diffusion-weighted Magnetic Resonance Imaging for the assessment of diminishing colorectal liver metastases by chemotherapy (DREAM study).
Dr. Nara conducts a multiinstitutional questionnaire study to evaluate the feasibility of preoperative CT to estimate TNM stage of biliary cancer in order to prepare for the future phase III study of preoperative chemotherapy for advanced biliary cancer.
Each staff attends three to four domestic or international academic meetings per year. Residents and chief residents also have opportunities to make a presentation with the assistance of staff surgeons.
Clinical trials
In addition to the above mentioned two RCTs (ND-trial and ESOP trial) and DREAM study, a uniinstitutional clinical trial to evaluate the R0 resection rate following preoperative SIROX therapy for borderline resectable pancreatic cancer is planned to be initiated in June 2018.
Education
Each resident attends one to two major HBP surgeries mainly as the first assistant. They also have the chance to be an operator depending on their skill. For each case, they learn how to decide the indication and type of procedure based on preoperative images. In the operation room, residents learn not only each step of HBP surgery, but also tips on how to help safely proceed with surgery. The chief resident trains them in a two-year program. In the first year, they devote themselves to the management of all inpatients and attend basically every surgery. Depending on the development of their skills, they have the opportunity to be an operating surgeon for major HBP surgery. In the second year, the chief resident works on research studies and publishes several English papers. Motivated residents also have the opportunity to make presentations in academic meetings and write English papers.
Visitors from both domestic and foreign institutions are welcome anytime.
Future prospects
HBP malignancy often requires technically demanding surgical procedures, whereas the long-term prognosis so far is not satisfactory. Our most important mission is to establish more safe and feasible surgical techniques including perioperative patient management, and to promote survival outcomes by multidisciplinary approaches. Due to the recent advances of chemotherapy, we have experienced a few patients who achieved curative surgical resection for initially unresectable pancreatic cancer due to local advancement. So the feasibility of conversion therapy should be assessed prospectively. We continue making efforts to create new skills and treatment strategies. In addition, clinical trials to explore unclarified clinical questions are expected.
List of papers published in January 2017 - March 2018
Journal
1. Iwao Y, Ojima H, Kobayashi T, Kishi Y, Nara S, Esaki M, Shimada K, Hiraoka N, Tanabe M, Kanai Y. Liver atrophy after percutaneous transhepatic portal embolization occurs in two histological phases: Hepatocellular atrophy followed by apoptosis. World journal of hepatology, 9:1227-1238, 2017
2. Iwasaki T, Nara S, Kishi Y, Esaki M, Shimada K, Hiraoka N. Surgical treatment of neuroendocrine tumors in the second portion of the duodenum: a single center experience and systematic review of the literature. Langenbecks Arch Surg, 402:925-933, 2017
3. Fukuoka K, Nara S, Honma Y, Kishi Y, Esaki M, Shimada K. Hepatectomy for Colorectal Cancer Liver Metastases in the Era of Modern Preoperative Chemotherapy: Evaluation of Postoperative Complications. World J Surg, 41:1073-1081, 2017
4. Hayashi H, Kohno T, Ueno H, Hiraoka N, Kondo S, Saito M, Shimada Y, Ichikawa H, Kato M, Shibata T, Morizane C, Sakamoto Y, Shimada K, Komatsu Y, Sakamoto N, Okusaka T. Utility of Assessing the Number of Mutated KRAS, CDKN2A, TP53, and SMAD4 Genes Using a Targeted Deep Sequencing Assay as a Prognostic Biomarker for Pancreatic Cancer. Pancreas, 46:335-340, 2017
5. Kishi Y, Nara S, Esaki M, Hiraoka N, Shimada K. Salvage hepatectomy for local recurrence of hepatocellular carcinomas offers survival comparable to that of matched patients who undergo primary hepatectomies. Eur J Surg Oncol, 43:1076-1082, 2017
6. Furukawa D, Chijiwa T, Matsuyama M, Mukai M, Matsuo EI, Nishimura O, Kawai K, Suemizu H, Nakagohri T, Ozawa S, Shimada K, Hiraoka N, Nakamura M. Plasma membrane expression of ZNF185 is a prognostic factor in pancreatic ductal carcinoma. Oncology letters, 14:3633-3640, 2017