Annual Report 2017
Supportive Care Development Center
Narikazu Boku, Emi Fujii, Naoko Inamura, Shiori Yamaoka, Mami Akutsu, Naoko Arii, Chihoko Hasegawa, Eriika Onuki, Momoko Takahashi, Kurumi Jo, Aya Fukuoka, Yasuko Abiru, Kiyomi Kawase, Miwako Saito
Introduction
During the treatment and management of cancer patients, because there are various unmet needs which cannot be satisfied and/or solved by each patient's attending physician alone, it is generally recognized that taking a team approach to these problems is very important. In September 2016, the Supportive Care Development Center was opened on the eighth floor of the hospital as the base of team medicine in the National Cancer Center Hospital (NCCH).
Our team and what we do
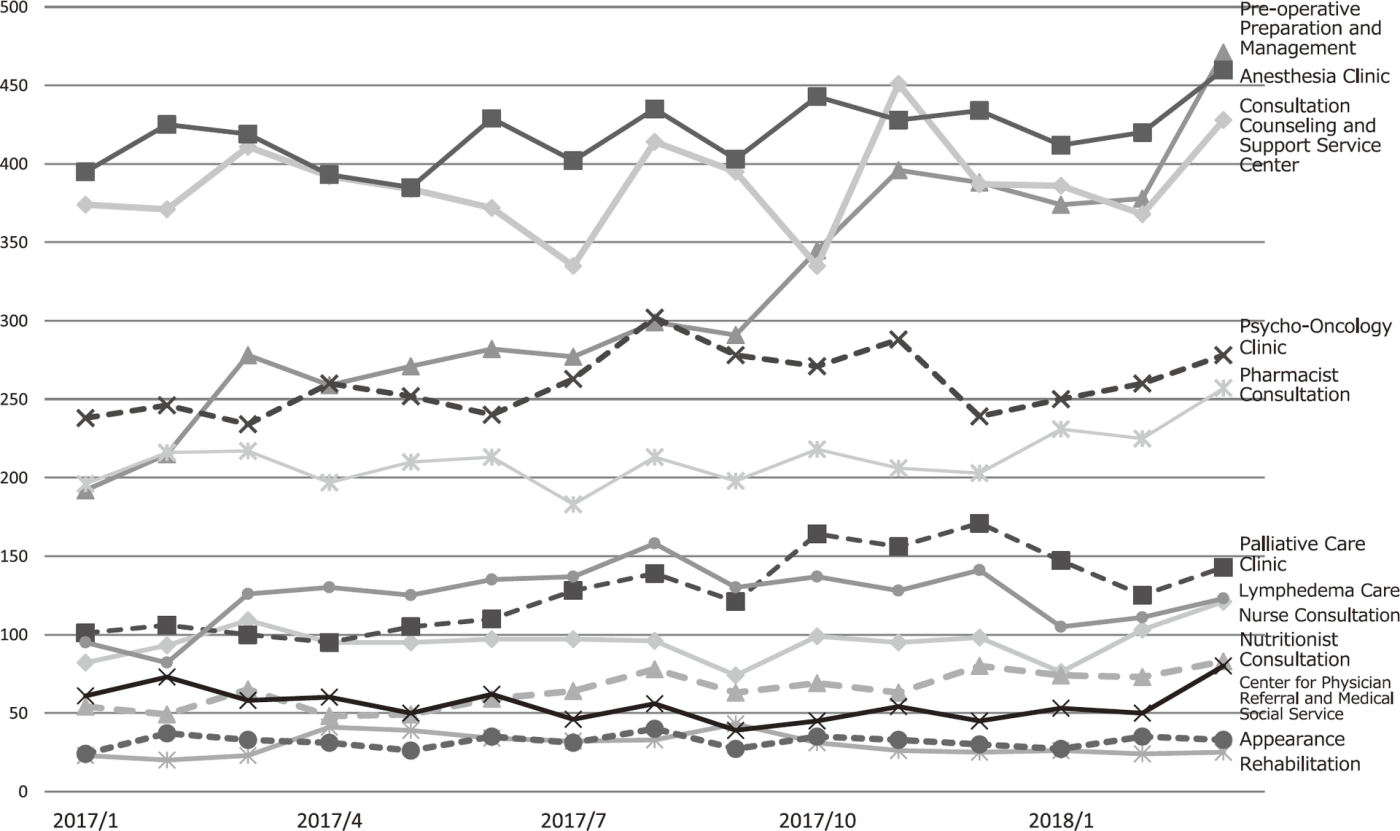
The standing programs have increased from six in 2016 to 12 in 2017: Nurse Consultation, Pre-operative Preparation and Management, Consultation Counseling and Support Service Center, Rehabilitation, Pharmacist Consultation, Nutritionist Consultation, Palliative Care Clinic, Psycho-Oncology Clinic, Anesthesia Clinic, Lymphedema Care, Appearance Center, and Center for Physician Referral and Medical Social Service. The numbers of patients participating in these programs from January 2017 to March 2018 were 95, 314, 387, 30, 212, 65, 127, 260, 419, 124, 32, 55 per months. Total number of patients visiting the Supportive Care Development Center has increased up to 128 per day, including other periodic classes and peer meetings such as Adolescents and Young Adults (AYA), Pain Control, Support for the Family of Pediatric Patients, Pancreato-biliary Cancer Patients, Chemotherapy, Body Image for Breast Cancer Patients, Relaxation and so on. On March 10 in 2017, "Exhibition of cancer patient care and device for daily life" was held to share information of patient care with patients and their families not only inside but also outside the NCCH.
Research activities
As the policy of the research in the Supportive Care Development Center, we recognize that continuous improvement in our activity is important for progression and hope that the know-how obtained from performing our programs can help the medical staff of other medical institutions taking care of cancer patients all over Japan. For this goal, we plan each program, do daily activity according to the pre-specified standard procedure, check the outcomes from patient's point of view and the costs (time), and take an action for further improvement (PDCA cycle). Actually, we have made checklists in the program of the pre-operative preparation and management and order the required laboratory tests or additional management. For the instruction of oral anti-tumoragents' administration by patients, we are preparing the interactive tool using iPad to evaluate the patients' understanding and the time used for explanation. This system is based on the cloud system, considering the availability in other hospitals. A protocol for the retrospective study evaluating each program at the Supportive Care Development Center has been approved. Now we are conducting several retrospective studies.
Education
Three nurses from three hospital wards participate in the nurse consultation and pre-operative management programs and receive on-the- job training under the supervision of the staff of the Supportive Care Development Center.
Future prospects
For each ongoing program, we will prepare a standard operation procedure and evaluate the outcome and spending time (cost). Considering the PDCA (plan-do-check-act) cycle method, we try to improve and newly develop our programs continuously and to be a model for other institutions taking care of cancer patients in Japan.
Table 1. The number of patients participating in each program in the Supportive Care Development Center