Annual Report 2018
Department of Thoracic Surgery
Masahiro Tsuboi, Keiju Aokage, Tomohiro Miyoshi, Kenta Tane, Takashi Sakai, Satoshi Okada, Shoko Nakasone
Introduction
The Department of Thoracic Surgery has three missions: surgical treatment, surgical resident training, and clinical research. Thoracic surgeries involve the treatment of thoracic neoplasms, primary and metastatic lung tumors, as well as mediastinal, pleural, and chest wall tumors. Our department specializes in the surgical treatment of pulmonary carcinomas. Routine surgical treatment modalities for carcinomas include limited resection (wedge or segmental resection) and simple resection (lobectomy or pneumonectomy) with or without systematic lymph node dissection. Thoracoscopic assistance is almost always used. Non-routine surgical procedures involve complex approaches such as broncho-/angio-plasty, combined resection with adjacent structures, and perioperative adjuvant treatment. Since its establishment in 1992, our department has been one of the most active leaders in the field of lung cancer in Japan. Moreover, it has been an active participant in international and national scientific venues. This year, in addition to 16 scientific papers published in English, our department made 30 presentations: four international, 23 national, and four regional.
The Team and What We Do
The Department of Thoracic Surgery is presently composed of four consultant surgeons including a chief and eight or nine residents. Our department has adopted a team approach in patient treatment and resident training. Potential surgical intervention candidate cases are presented every Tuesday evening at a multidisciplinary team conference of thoracic surgeons, oncology physicians, radiologists, and residents.
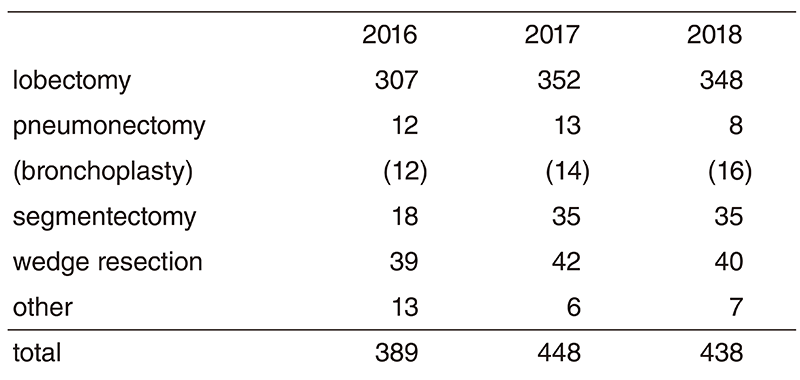
Each case is thoroughly and vigorously reviewed and discussed. To improve the English fluency of staff members and residents in preparation for international presentations, and to better involve visiting physicians from other countries, treatment modality discussions are conducted in English. Moreover, selected patients' records are radiologically and cytopathologically reviewed every Friday morning. These reviews aim to improve the interpretation of radiologic indications to pathology findings, accurately evaluate surgical indications, and upgrade knowledge on rare histologies. We believe that these activities improve the knowledge base, treatment indications, and surgical treatment. For non-small cell histology, primary pulmonary carcinomas in clinical stages I/II and IIIA without bulky or multistation-involved mediastinal nodes, and primary pulmonary small cell carcinomas in clinical stage I, surgical resection is indicated as a cure. Optimum treatment modalities are being sought via clinical trials with the aim of improving the poor prognosis of patients with bulky or clinically and histologically proven multistation mediastinal lymph node metastases, with disease invading the neighboring vital structures, or with small cell cancers in clinical stage II and later. Resection of metastatic lung tumor is attempted based on modified Thomfold's criteria after consultation with the patient. The majority of these cases are metastases from colorectal carcinomas, while most of the mediastinal tumors are thymic epithelial tumors. The surgical procedures of the Department of Thoracic Surgery have generally remained similar for the past decade, but we have employed portaccess thoracoscopic surgery more often for the last several years. Approximately 20% of the surgeries are completed via a 3-port access, and 70% of the surgeries are video-thoracoscopically assisted. To date, the average postoperative hospital stay of patients in our department has been improved and become shorter, three days being the shortest with a median of seven days for cases of primary lung cancer. These shorter hospital stays are achieved with a slightly better complication rate than the normal rate. This year, 30-day operative mortality occurred in three patients undergoing surgery for primary lung cancer.
Research activities
Research in the area of combined treatment, especially immunotherapy, has now advanced to clinical trials. It is the goal for researchers in our department to acquire a basic understanding of the cellular and molecular mechanisms leading to the development and progression of lung cancer and apply these findings to further the development of immunotherapy-based prevention and treatment strategies.
Clinical trials
There are the following prospective trials in this department.
1) Primary investigator and a member of an organized trial of TS-1 vs. UFT adjuvant chemotherapy for completely resected pathologic stage I (> 2 cm) non-small cell lung cancer [JCOG 0707, phase III, patient accrual completed].
2) Primary investigator and a member of an organized trial of sublobar resection for peripheral GGO dominant cT1aN0M0 lung adenocarcinomas [JCOG 0804, phase II, patient accrual completed].
3) Study coordinator and a member of an organized trial of segmental resection vs. lobectomy for peripheral T1aN0M0 non-small cell lung cancers [JCOG 0802, phase III, patient accrual completed].
4) Study coordinator and a member of an organized trial of sublobar resection for peripheral GGO dominant cT1bN0M0 lung adenocarcinomas [JCOG 1211, phase III, patient accrual completed]
5) Primary investigator and a member of an organized trial of Cisplatin/Pemetrexed vs. Cisplatin/Vinorelbine adjuvant chemotherapy for completely resected pathologic stage II-IIIA non-small cell lung cancer [JIPANG, phase III, the first presentation will be made in 2019].
6) A member of an organized trial of the therapeutic significance of lobe-specific lymph node dissection compared with the systematic lymph node dissection for clinical stage I-II NSCLC [JCOG1413, phase III patient accrual is ongoing]
7) A member of an organized trial of the utility of the sub-lobar resection for clinical stage I NSCLC with idiopathic pulmonary fibrosis [JCOG1708, phase III, patient accrual ongoing]
8) A member of an organized trial of Human Atrial Natriuretic Peptide during perioperative period for completed resectable non-small cell lung cancer [JANP, randomized phase II, patient accrual ongoing].
9) A member of an organized trial of postoperative maintenance adjuvant immunotherapy with S-588410 for completed resected stage II-IIIA non-small cell lung cancer [S-588410, phase II, patient accrual ongoing]
In addition, four corporate trials are participating.
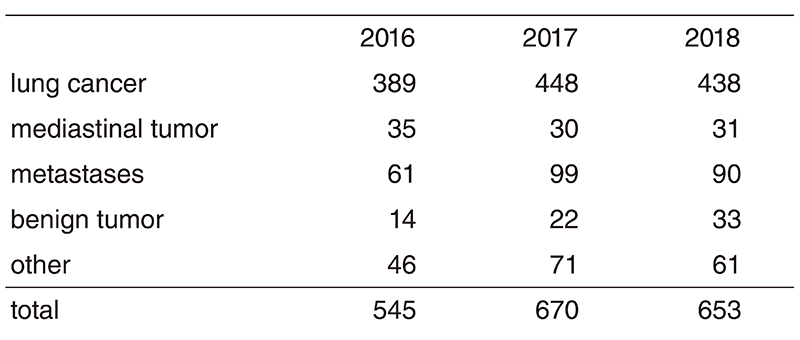
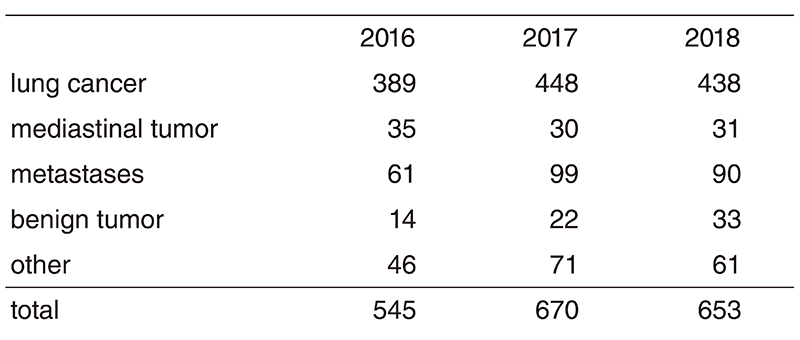
Education
Our training program is to educate residents by expanding their knowledge and technical skills in the treatment of lung cancer, other thoracic malignancies, and benign tumors, such as hamartoma and mediastinal cystic lesions. In addition, we seek to instill in the trainee a desire for continued introspection and self-education, open communication between all health care providers, while maintaining a respectful and professional demeanor. (Table 1, Table 2)
Table 1. Number of surgically resected patients
Future prospects
Treatment advances in thoracic cancers including lung, mesothelioma, thymic malignancies and lung metastases have been slow to develop, even though these cancers are among the most common clinical problems. This clinical and laboratory research is vital to making progress.
List of papers published in 2018
Journal
1. Navani N, Fisher DJ, Tierney JF, Stephens RJ, Burdett S. The Accuracy of Clinical Staging of Stage I-IIIa Non-Small Cell Lung Cancer: An Analysis Based on Individual Participant Data. Chest, 155:502-509, 2019
2. Yoh K, Takamochi K, Shukuya T, Hishida T, Tsuboi M, Sakurai H, Goto Y, Yoshida K, Ohde Y, Okumura S, Ohashi Y, Kunitoh H. Pattern of care in adjuvant therapy for resected Stage I non-small cell lung cancer: real-world data from Japan. Jpn J Clin Oncol, 49:63-68, 2019
3. Miyashita T, Omori T, Nakamura H, Sugano M, Neri S, Fujii S, Hashimoto H, Tsuboi M, Ochiai A, Ishii G. Spatiotemporal characteristics of fibroblasts-dependent cancer cell invasion. J Cancer Res Clin Oncol, 145:373-381, 2019
4. Miyoshi T, Yoshida J, Aokage K, Tane K, Ishii G, Tsuboi M. Stapling cartridge lavage cytology in limited resection for pulmonary malignant tumors: assessment of cytological status of the surgical margin. Heliyon, 5:e01240, 2019
5. Katsumata S, Aokage K, Nakasone S, Sakai T, Okada S, Miyoshi T, Tane K, Hayashi R, Ishii G, Tsuboi M. Radiologic Criteria in Predicting Pathologic Less Invasive Lung Cancer According to TNM 8th Edition. Clin Lung Cancer, 20:e163-e170, 2019
6. Sekihara K, Aokage K, Oki T, Omori T, Katsumata S, Ueda T, Miyoshi T, Goto M, Nakasone S, Ichikawa T, Hishida T, Yoshida J, Hisakane K, Goto K, Tsuboi M. Long-term survival after complete resection of non-small-cell lung cancer in patients with interstitial lung disease. Interact Cardiovasc Thorac Surg, 26:638-643, 2018
7. Ichikawa T, Aokage K, Sugano M, Miyoshi T, Kojima M, Fujii S, Kuwata T, Ochiai A, Suzuki K, Tsuboi M, Ishii G. The ratio of cancer cells to stroma within the invasive area is a histologic prognostic parameter of lung adenocarcinoma. Lung Cancer, 118:30- 35, 2018
8. Nakasone S, Mimaki S, Ichikawa T, Aokage K, Miyoshi T, Sugano M, Kojima M, Fujii S, Kuwata T, Ochiai A, Tsuboi M, Goto K, Tsuchihara K, Ishii G. Podoplanin-positive cancer-associated fibroblast recruitment within cancer stroma is associated with a higher number of single nucleotide variants in cancer cells in lung adenocarcinoma. J Cancer Res Clin Oncol, 144:893-900, 2018
9. Makinoshima H, Umemura S, Suzuki A, Nakanishi H, Maruyama A, Udagawa H, Mimaki S, Matsumoto S, Niho S, Ishii G, Tsuboi M, Ochiai A, Esumi H, Sasaki T, Goto K, Tsuchihara K. Metabolic Determinants of Sensitivity to Phosphatidylinositol 3-Kinase Pathway Inhibitor in Small-Cell Lung Carcinoma. Cancer Res, 78:2179-2190, 2018
10. Yamazaki S, Higuchi Y, Ishibashi M, Hashimoto H, Yasunaga M, Matsumura Y, Tsuchihara K, Tsuboi M, Goto K, Ochiai A, Ishii G. Collagen type I induces EGFR-TKI resistance in EGFR-mutated cancer cells by mTOR activation through Akt-independent pathway. Cancer Sci, 109:2063-2073, 2018
11. Wu YL, Herbst RS, Mann H, Rukazenkov Y, Marotti M, Tsuboi M. ADAURA: Phase III, Double-blind, Randomized Study of Osimertinib Versus Placebo in EGFR Mutation-positive Early-stage NSCLC After Complete Surgical Resection. Clin Lung Cancer, 19:e533-e536, 2018
12. Sakai T, Tane K, Usui Y, Miyoshi T, Matsumoto S, Aokage K, Goto K, Suzuki M, Ishii G, Tsuboi M. Utility of Site-Specific Biopsy for Diagnosis of Desmoplastic Malignant Mesothelioma. Ann Thorac Surg, 106:e125-e128, 2018
13. Hishida T, Aokage K, Yoshida J, Miyoshi T, Tsuboi M. Extended bronchoplasty for locally advanced left lower lobe lung cancer: surgical technique and outcomes. Interact Cardiovasc Thorac Surg, 27:602-605, 2018
14. Katsumata S, Aokage K, Miyoshi T, Tane K, Nakamura H, Sugano M, Kojima M, Fujii S, Kuwata T, Ochiai A, Hayashi R, Tsuboi M, Ishii G. Differences of tumor microenvironment between stage I lepidic-positive and lepidic-negative lung adenocarcinomas. J Thorac Cardiovasc Surg, 156:1679-1688.e2, 2018
15. Kanai R, Tane K, Ishii G, Suzuki J, Sakai T, Okada S, Miyoshi T, Aokage K, Tsuboi M. Clinical prediction of solitary pulmonary nodule after a curative resection for gastric cancer. Jpn J Clin Oncol, 48:1083-1087, 2018
16. Sakai T, Aokage K, Neri S, Nakamura H, Nomura S, Tane K, Miyoshi T, Sugano M, Kojima M, Fujii S, Kuwata T, Ochiai A, Iyoda A, Tsuboi M, Ishii G. Link between tumor-promoting fibrous microenvironment and an immunosuppressive microenvironment in stage I lung adenocarcinoma. Lung Cancer, 126:64-71, 2018
17. Eckert CE, Harris JL, Wong JB, Thompson S, Kassis ES, Tsuboi M, Ott HC, Force S. Preclinical quantification of air leaks in a physiologic lung model: effects of ventilation modality and staple design. Med Devices (Auckl), 11:433-442, 2018
18. Ueda T, Aokage K, Mimaki S, Tane K, Miyoshi T, Sugano M, Kojima M, Fujii S, Kuwata T, Ochiai A, Kusumoto M, Suzuki K, Tsuchihara K, Nishikawa H, Goto K, Tsuboi M, Ishii G. Characterization of the tumor immune-microenvironment of lung adenocarcinoma associated with usual interstitial pneumonia. Lung Cancer, 126:162-169, 2018
19. Ueda T, Aokage K, Nishikawa H, Neri S, Nakamura H, Sugano M, Tane K, Miyoshi T, Kojima M, Fujii S, Kuwata T, Ochiai A, Kusumoto M, Suzuki K, Tsuboi M, Ishii G. Immunosuppressive tumor microenvironment of usual interstitial pneumonia-associated squamous cell carcinoma of the lung. J Cancer Res Clin Oncol, 144:835-844, 2018
20. Aokage K, Miyoshi T, Ishii G, Kusumoto M, Nomura S, Katsumata S, Sekihara K, Tane K, Tsuboi M. Influence of Ground Glass Opacity and the Corresponding Pathological Findings on Survival in Patients with Clinical Stage I Non-Small Cell Lung Cancer. J Thorac Oncol, 13:533-542, 2018
