Annual Report 2018
Department of Esophageal Surgery
Hiroyuki Daiko, Junya Oguma, Jun Kanamori, Koshiro Ishiyama, Yuki Hirano, Daisuke Kurita
Introduction
The Department of Esophageal Surgery deals with neoplasms arising from the esophagus. The surgical management of esophageal cancer has been the main clinical research activity of this department. In particular, our department is striving to establish minimally invasive surgery that consists of neoadjuvant treatment followed by minimally invasive esophagectomy. Our department is conducting a study to define the role of surgery in the multimodal approach to the treatment of esophageal cancer, and is aiming for thoracolaparoscopic esophagectomy, which consists of thoracoscopic esophagectomy and laparoscopic reconstruction, to become a standard surgical procedure.
The Team and What We Do
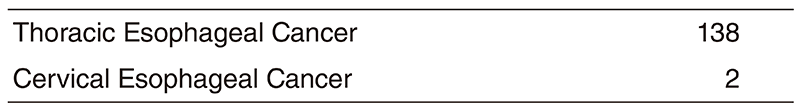
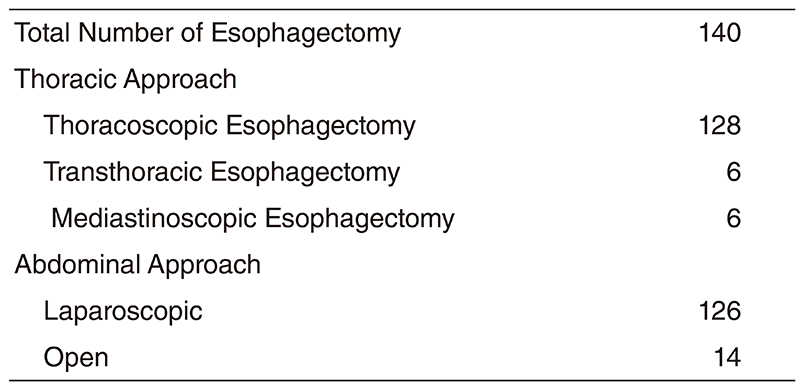
The Department of Esophageal Surgery consists of three staff surgeons and three residents. An Esophageal Conference is held every Tuesday evening to discuss the diagnosis, staging, and treatment strategy for each patient and is attended by surgeons, medical oncologists, endoscopists, radiologists, radiation oncologists, and head & neck surgeons. Approximately four patients are operated upon every week. In 2018, 142 patients underwent esophagectomies, including 140 cases of thoracic esophageal cancer and two cases of cervical cancer. Transthoracic esophagectomies with extended lymph node dissection were performed on six cases. Thoracoscopic esophagectomies in the prone position with radical lymph node dissection were undertaken in 128 cases. Mediastinoscopic esophagectomy for patients above 80 or patients with multiple complications was undertaken in six cases. Postoperatively, within 30 days, three patients died due to complications after a salvage operation.
Research Activities
Currently, our department is examining the role of thoracolaparoscopic esophagectomy as a minimally invasive esophagectomy that consists of thoracoscopic esophagectomy and laparoscopic reconstruction. For patients without radical chemoradiotherapy, thoracoscopic esophagectomy in the prone position with radical lymph node dissection and laparoscopic reconstruction after esophagectomy for patients without a history of laparotomy are being attempted to become a standard surgical procedure for esophageal cancer.
For treating patients aged over 80 years or at high risk, a two-stage surgical procedure divided into resection and reconstruction is being attempted.
A Phase III study of tri-modality combination therapy with induction docetaxel, cisplatin, 5-fluorouracil (DCF) vs definitive chemoradiotherapy (dCRT) for locally advanced unresectable squamous cell carcinoma of the thoracic esophagus (JCOG1510, TRIANgLE trial) is ongoing.
A randomized controlled phase III study of minimally invasive versus open esophagectomy for thoracic esophageal cancer (JCOG1409, MONET trial) is ongoing.
Since 2000, our department has started to perform salvage surgery for patients in whom definitive chemoradiotherapy has failed. The operative procedures and postoperative management have been refined gradually. Our department is also studying the role and efficacy of salvage surgery in the multimodal treatment of esophageal cancer.
List of papers published in 2018
Journal
1. Hashimoto J, Kato K, Ito Y, Kojima T, Akimoto T, Daiko H, Hamamoto Y, Matsushita H, Katano S, Hara H, Tanaka Y, Saito Y, Nagashima K, Igaki H. Phase II feasibility study of preoperative concurrent chemoradiotherapy with cisplatin plus 5-fluorouracil and elective lymph node irradiation for clinical stage II/III esophageal squamous cell carcinoma. Int J Clin Oncol, 24:60-67, 2019
2. Sato T, Fujita T, Fujiwara H, Daiko H. Internal hernia to the retrosternal space is a rare complication after minimally invasive esophagectomy: three case reports. Surg Case Rep, 5:26, 2019
3. Fujita T, Sato T, Sato K, Hirano Y, Fujiwara H, Daiko H. Clinical manifestation, risk factors and managements for postoperative chylothorax after thoracic esophagectomy. J Thorac Dis, 11:S198-S201, 2019
4. Wada S, Inoguchi H, Sadahiro R, Matsuoka YJ, Uchitomi Y, Sato T, Shimada K, Yoshimoto S, Daiko H, Shimizu K. Preoperative Anxiety as a Predictor of Delirium in Cancer Patients: A Prospective Observational Cohort Study. World J Surg, 43:134-142, 2019
5. Nishiumi S, Fujigaki S, Kobayashi T, Kojima T, Ito Y, Daiko H, Kato K, Shoji H, Kodama Y, Honda K, Yoshida M. Metabolomics-based Discovery of Serum Biomarkers to Predict the Side-effects of Neoadjuvant Chemoradiotherapy for Esophageal Squamous Cell Carcinoma. Anticancer Res, 39:519-526, 2019
6. Fujigaki S, Nishiumi S, Kobayashi T, Suzuki M, Iemoto T, Kojima T, Ito Y, Daiko H, Kato K, Shouji H, Honda K, Azuma T, Yoshida M. Identification of serum biomarkers of chemoradiosensitivity in esophageal cancer via the targeted metabolomics approach. Biomark Med, 12:827-840, 2018
7. Nozaki I, Mizusawa J, Kato K, Igaki H, Ito Y, Daiko H, Yano M, Udagawa H, Nakagawa S, Takagi M, Kitagawa Y. Impact of laparoscopy on the prevention of pulmonary complications after thoracoscopic esophagectomy using data from JCOG0502: a prospective multicenter study. Surg Endosc, 32:651-659, 2018
8. Koyanagi K, Kato F, Kanamori J, Daiko H, Ozawa S, Tachimori Y. Clinical significance of esophageal invasion length for the prediction of mediastinal lymph node metastasis in Siewert type II adenocarcinoma: A retrospective single-institution study. Ann Gastroenterol Surg, 2:187-196, 2018
9. Komatsu H, Watanuki S, Koyama Y, Iino K, Kurihara M, Uesugi H, Yagasaki K, Daiko H. Nurse Counseling for Physical Activity in Patients Undergoing Esophagectomy. Gastroenterol Nurs, 41:233-239, 2018
10. Kato F, Monma S, Koyanagi K, Kanamori J, Daiko H, Igaki H, Tachimori Y. Long-term outcome after resection for recurrent oesophageal cancer. J Thorac Dis, 10:2691-2699, 2018
11. Okada N, Fujita T, Kanamori J, Sato A, Horikiri Y, Sato T, Fujiwara H, Daiko H. A case report of postoperative VRSA enteritis: Effective management of rifampicin for vancomycin resistant Staphylococcus aureus enteritis after esophagectomy and colon reconstruction. Int J Surg Case Rep, 52:75-78, 2018
12. Fujiwara H, Kanamori J, Nakajima Y, Kawano T, Miura A, Fujita T, Akita K, Daiko H. An anatomical hypothesis: a "concentric-structured model" for the theoretical understanding of the surgical anatomy in the upper mediastinum required for esophagectomy with radical mediastinal lymph node dissection. Dis Esophagus, 2018
13. Tamaoki M, Komatsuzaki R, Komatsu M, Minashi K, Aoyagi K, Nishimura T, Chiwaki F, Hiroki T, Daiko H, Morishita K, Sakai Y, Seno H, Chiba T, Muto M, Yoshida T, Sasaki H. Multiple roles of single-minded 2 in esophageal squamous cell carcinoma and its clinical implications. Cancer Sci, 109:1121-1134, 2018
14. Kadota T, Hatogai K, Yano T, Fujita T, Kojima T, Daiko H, Fujii S. Pathological tumor regression grade of metastatic tumors in lymph node predicts prognosis in esophageal cancer patients. Cancer Sci, 109:2046-2055, 2018
15. Sato T, Fujita T, Okada N, Fujiwara H, Kojima T, Hayashi R, Daiko H. Postoperative pulmonary complications and thoracocentesis associated with early versus late chest tube removal after thoracic esophagectomy with three-field dissection: a propensity score matching analysis. Surg Today, 48:1020-1030, 2018
