Annual Report 2019
Department of Breast Surgery
Tatsuya Onishi, Tsuguo Iwatani, Takamichi Yokoe
Introduction
We treat patients with operable malignant mammary glands. Diagnosis of breast disease, surgical treatment and follow-up for breast cancer patients are our main professional practices. The Department of Breast Surgery is committed to providing the latest, most comprehensive breast treatments for our patients. The multidisciplinary approach to the diagnosis and treatment of cancer is carried out under cooperation among related specialists.
Our department mainly focuses on “minimally invasive surgery” and performs a thorough investigation for an oncologically safe approach, less morbidity and good cosmesis. For example, although sentinel lymph node (SLN) biopsy has already been established as the standard care for clinical node negative patients, omitting axillary lymph node dissection (ALND) for positive SLNs has started in clinical practice as an expanded indication. On the other hand, preoperative systemic therapy provides the opportunity for a curative operation or breast-conserving surgery to avoid mastectomy. Moreover, we can provide breast reconstructive surgery in collaboration with the Department of Plastic and Reconstructive Surgery. These procedures will contribute to a better quality of life for patients with breast cancer.
The Team and What We Do
For the regular activities of our department, a daily morning routine round is scheduled for inpatients by all staff. Moreover, our weekly preoperative diagnostic imaging conference is conducted to discuss the surgical treatment planning for each patient. A clinical conference to decide on courses of treatment by multidisciplinary breast care team members is held twice a month. A monthly pathological conference on breast cancer is also conducted. At those conferences, individual cases are presented to a team of highly trained cancer specialists, including radiologists, breast surgeons, pathologists, radiation oncologists, and medical oncologists. Our multidisciplinary team approach to breast cancer treatment provides superior-quality care to patients.
Changes in the annual number of patients with breast cancer who underwent surgery are shown in Table 1. A total of 413 patients with primary breast cancer and 49 patients with recurrence or another breast disease were operated on.
Table 1. Number of patients (April, 2019 - March, 2020)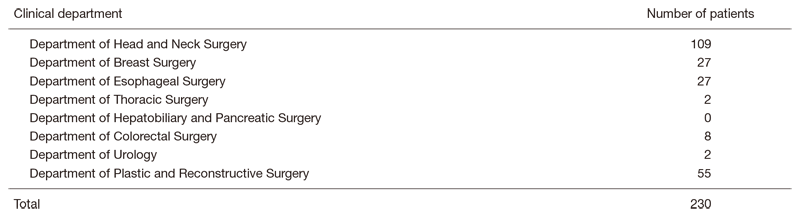
Total mastectomy with immediate breast reconstruction was performed in 29 patients. BP: partial mastectomy, BT: total mastectomy, SNB: sentinel node biopsy, ALND: axillary lymph node dissection, RFA: radio frequency ablation, DIEP: deep Inferior Epigastric Perforator flap, LD: latissimus dorsi muscle transfer flap, TE: tissue Expander
Hospital East
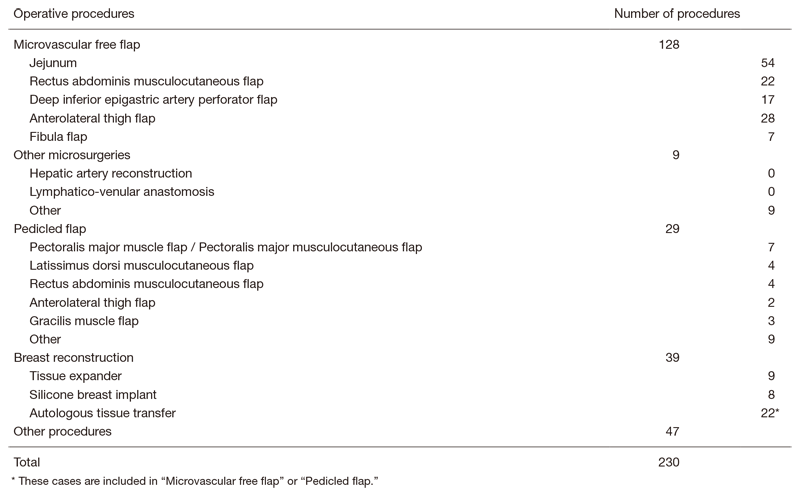
Sixteen immediate breast reconstruction surgeries were included. Of the patients with primary breast cancer, 68 (16%) underwent primary systemic therapy. The types and number of operative procedures performed in 2019 are shown in Table 2. The rate of breast-conserving surgery was 39% (163/413). Sentinel node biopsy was performed in 332 patients, and 310 patients were spared from ALND. The number of immediate breast reconstruction surgeries using tissue expanders decreased compared to 2018, because the tissue expanders were recalled due to breast implant-associated anaplastic large cell lymphoma.
Table 2. Operative procedures (April, 2019 - March, 2020)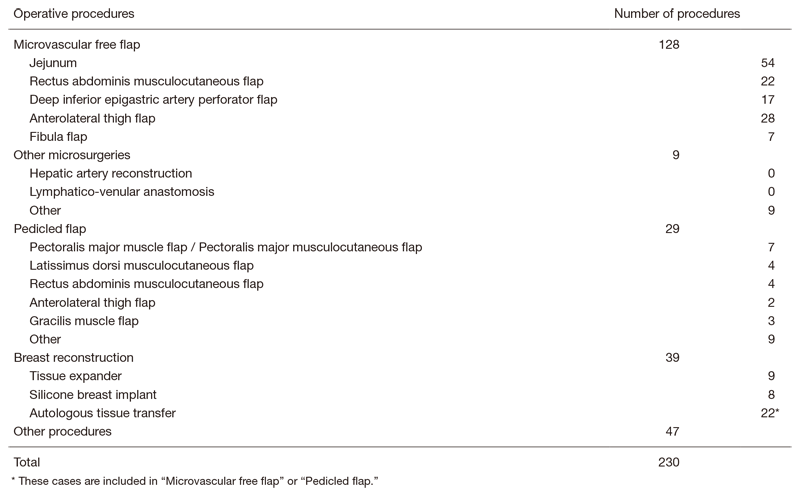
Research activities
We contribute to the establishment of new standard treatment for breast cancer patients by actively enrolling participants in clinical trials. The clinical trials we are currently conducting are as follows.
Clinical trials
1) Single-arm confirmatory trial of endocrine therapy alone for estrogen receptor-positive, low-risk ductal carcinoma in situ of the breast (JCO1505, LORETTA Trial): This is a single arm interventional study to confirm whether endocrine therapy alone for ER-positive low-risk DCIS is safe and effective compared with the current standard treatment.
2) Study of avoiding mastectomy using trastuzumab, pertuzumab and radiation for breast cancer (JCOG1806, AMATERAS-BC): This is single arm study to confirm the efficacy of avoiding surgical treatment for HER2-positivebreast cancer patients who received neoadjuvant chemotherapy and achieved complete response.
3) Estimation of willingness to pay for breast cancer treatments through contingent valuation method in Japanese breast cancer patients (JCOG1709A): This is a prospective observational study to elucidate how Japanese breast cancer patients consider the financial value for their life and health by using the contingent valuation method, prospectively.
4) Radiofrequency ablation (RFA) using a Cool-tip electrode system (RAFAELO study): A phase II study on RFA without resection was performed for T=<1.5 cm, N0 breast cancer patients using a Cool-tip electrode system.
5) Effectiveness of primary tumor resection for metastatic breast cancer (JCOG 1017): In this clinical trial, the primary tumor resection plus systemic therapy arm is compared to the systemic therapy alone arm in metastatic breast cancer.
6) Intensive vs. standard post-operative surveillance in high-risk breast cancer patients (JCOG1204, INSPIRE Trial): This is a randomized phase III trial to confirm the superiority of intensive follow-up to standard follow-up in terms of overall survival in high-risk breast cancer patients.
7) Clinical benefit of treatment after trastuzumab-emtansine for HER2-positive metastatic breast cancer: A real-world multicenter cohort study in Japan (WJOG12519B): The aim of his study is to evaluate real-world treatment choice and efficacy of treatments after T-DM1 for HER2-positive metastatic breast cancer.
Education
Targets of our education are to raise knowledge about breast disease, and to improve operative techniques.
Future prospects
We want to deliver the appropriate postoperative follow-up care, which has been a longtime concern in breast cancer medical care. We also aim at more operative development with minimally invasive and cosmetic surgery. Moreover, we will construct an evaluation axis from the patients' viewpoint for the cost effectiveness of clinical trials to establish standard treatments for breast cancer.
List of papers published in 2019
Journal
1. Yokoe T, Sato M, Yahagi M, Dogru M, Fujisaki H, Ogura M, Kawamata H, Asahara F, Takayama S, Harada H, Tanaka Y, Miyauchi J, Matsui J. Heterochronous Suture Line Recurrences in the Jejunal Pouch following Total Gastrectomy for Stage II Gastric Cancer: A Case Report and Literature Review. Case Rep Oncol, 13:225-232, 2020
2. Nakashoji A, Hayashida T, Kawai Y, Kikuchi M, Watanuki R, Yokoe T, Seki T, Takahashi M, Miyao K, Yamaguchi S, Kitagawa Y. Identification of a Modified HOXB9 mRNA in Breast Cancer. J Oncol, 2020:6065736, 2020
3. Kojima Y, Yoshie R, Kawamoto H, Shimo A, Uejima T, Iwatani T, Motoyoshi A, Kanemaki Y, Boku N, Tsugawa K. Trastuzumab Emtansine (T-DM1) Plus S-1 in Patients with Trastuzumab-Pretreated HER2-Positive Advanced or Metastatic Breast Cancer: A Phase Ib Study. Oncology, 96:309-317, 2019
4. Yokoe T, Hayashida T, Nagayama A, Nakashoji A, Maeda H, Seki T, Takahashi M, Takano T, Abe T, Kitagawa Y. Effectiveness of Antiemetic Regimens for Highly Emetogenic Chemotherapy-Induced Nausea and Vomiting: A Systematic Review and Network Meta-Analysis. Oncologist, 24:e347-e357, 2019
5. Watanuki R, Hayashida T, Kawai Y, Kikuchi M, Nakashoji A, Yokoe T, Toyota T, Seki T, Takahashi M, Kitagawa Y. Optimal use of anthracycline-free perioperative chemotherapy in HER2-positive breast cancer patients. Int J Clin Oncol, 24:807-814, 2019
6. Onishi T, Matsuda S, Nakamura Y, Kuramoto J, Tsuruma A, Sakamoto S, Suzuki S, Fuchimoto D, Onishi A, Chikaki S, Kaneko M, Kuwahata A, Sekino M, Yasuno H, Hanyu N, Kurita T, Takei H, Sakatani T, Taruno K, Nakamura S, Hayashida T, Jinno H, Kusakabe M, Handa H, Kameyama K, Kitagawa Y. Magnetically Promoted Rapid Immunofluorescence Staining for Frozen Tissue Sections. J Histochem Cytochem, 67:575-587, 2019
