Annual Report 2019
Department of Hepatobiliary and Pancreatic Surgery
Naoto Gotohda, Shinichiro Takahashi, Shin Kobayashi, Motokazu Sugimoto, Masaru Konishi, Masashi Kudo, Toshiyuki Suzuki, Ryo Morisue, Masatake Taniguchi, Sho Yasuta, Naoki Yagi, Ryuji Komine, Yusuke Abe, Tatsuki Ishikawa, Kimimasa Sasaki, Yu Shibahara, Kento Mishima
Introduction
The Department of Hepatobiliary and Pancreatic Surgery consists of five staff surgeons, three senior residents and nine junior resident surgeons. Our department is responsible for the surgical treatment of patients with hepatic, biliary, and pancreatic cancer and duodenal cancer or low-grade malignant tumors. We conduct multidisciplinary treatment in cooperation with the Department of Hepatobiliary and Pancreatic Oncology, the Department of Diagnostic Radiology and the Department of Radiation Oncology. We also conduct less invasive surgery: laparoscopic surgery for patients with liver cancer and pancreatic cancer.
The Team and What We Do
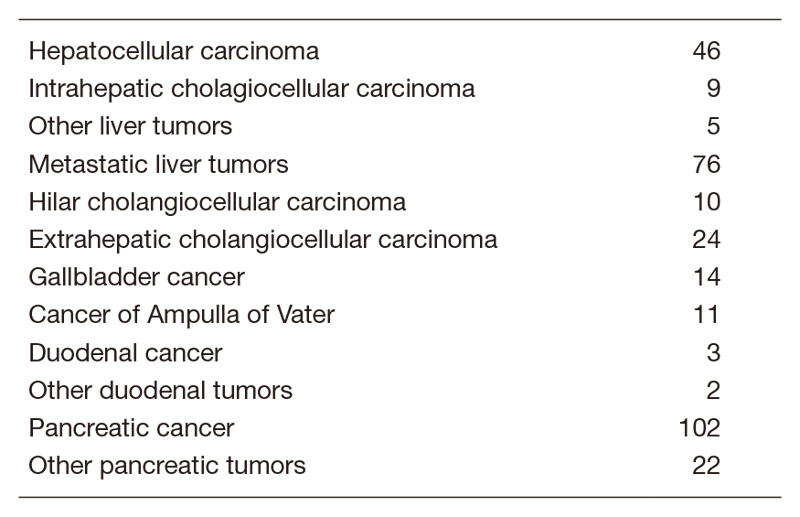
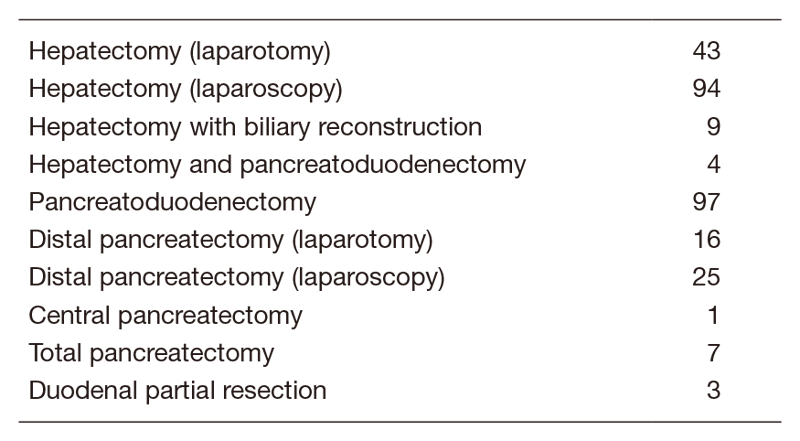
We work with outpatients five days a week and have about 20 inpatients. Staff meetings in which we discuss the treatment strategy or the points of surgery for patients are held with staff in the Department of Hepatobiliary and Pancreatic Oncology triweekly. The Cancer Board is held in cooperation with radiologists and medical oncologists every Tuesday. The pathology conference is held with pathologists every month. In 2019, 347 patients with hepatobiliary and pancreatic diseases underwent surgical treatment. The main diseases are shown in Table 1. Compared with the number of patients in 2018, the number of patients undergoing surgery in our department increased (Table 2). Laparoscopic surgery for the hepatobiliary and pancreatic surgical field is also expanding rapidly in Japan. We also performed a lot of laparoscopic surgical cases of hepatectomy (Lap-H) and distal pancreatectomy in 2019. We are establishing the position of the leading hospitals regarding Lap-H and organizing Lap-H seminars in our hospital to generalize the safe procedure of Lap-H.
Research activities
- Conversion surgery for pancreatic cancer
Currently, the treatment outcomes of pancreatic cancer patients are improving remarkably with the chemotherapy regimen Gem+nab-PTX or FOLFIRINOX. We try to perform conversion surgery for selected patients with borderline resectable or unresectable pancreatic cancer who received chemotherapy. We are currently evaluating good indications for conversion surgery. - Function-preserving surgery
Pancreas sparing duodenectomy (PSD) represents an alternative procedure to pancreaticoduodenectomy (PD) for patients with duodenal neoplasms. PSD is a less invasive procedure and has the advantage over PD of preservation of the pancreas. We are trying to establish a safe procedure for PSD. - Evaluation of the liver function
Postoperative liver failure is one of the fatal complications after major hepatectomy. We usually evaluate the liver function using the test of Indocyanine green retention rate at 15 min (ICG15). We are developing an alternative evaluation of the liver function using liver-specific magnetic resonance imaging (MRI) with the contrast agent of Gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid (Gd-EOB-DTPA) instead of using the test of ICG15.
Clinical trials
- A Phase III trial of S-1 versus observation in patients with resected biliary tract cancer (JCOG1202). Recruitment finished in 2018.
- Randomized phase II trial of chemoradiotherapy with S-1 versus gemcitabine and S-1 combination therapy as neoadjuvant treatment in patients with resectable pancreatic cancer (JASPAC04). Recruitment started in 2014.
- Non-randomized controlled study comparing proton beam therapy and hepatectomy for resectable hepatocellular carcinoma (JCOG1315C). Recruitment started in 2016.
- Japanese trial – A global study to evaluate the potential benefit of adjuvant chemotherapy for small bowel adenocarcinoma (JCOG1502C). Recruitment started in 2017.
- Comparison of Berizym and Pancrelipase for the effect of suppressing onset of hepatic seatosis after pancreaticoduodenectomy (ESOP Trial). Recruitment started in 2016.
- Randomized phase II/III study of gemcitabine and nab-paclitaxel therapy versus S-1 and concurrent radiotherapy as neoadjuvant treatment for borderline resectable pancreatic cancer (GABARNANCE Trial). Recruitment started in 2017.
- Investigator-Initiated Clinical Trial of Nivolumab Monotherapy and Subsequent Radical Surgery Following Preoperative Chemoradiotherapy in Patients with Microsatellite Stable Locally Advanced Rectal Cancer (EPOC 1504). Recruitment started in 2018.
Education
The ‘Board-certified expert surgeon’ is a high level of skill in the field of Hepatobiliary-pancreatic surgery. To be qualified as a board-certified surgeon, surgeons are required to perform a prescribed number of operations under the guidance of a board-certified instructor. The residents of our department are being trained to get the certifications by the end of the chief resident course. One senior resident (Dr. Kudo) passed the examination of a board-certified surgeon in 2019. We could first have a successful applicant during a senior residency.
Future prospects
The establishment of multidisciplinary treatment for patients with refractory hepatobiliary and pancreatic cancer and the establishment of less invasive surgery for patients with pancreatic cancer and liver cancer is our goal.
List of papers published in 2019
Journal
1. Ohtsuka T, Nakamura M, Hijioka S, Shimizu Y, Unno M, Tanabe M, Nagakawa Y, Takaori K, Hirono S, Gotohda N, Kimura W, Ito K, Katanuma A, Sano T, Urata T, Kita E, Hanada K, Tada M, Aoki T, Serikawa M, Okamoto K, Isayama H, Gotoh Y, Ishigami K, Yamaguchi H, Yamao K, Sugiyama M, Okazaki K. Prediction of the Probability of Malignancy in Mucinous Cystic Neoplasm of the Pancreas With Ovarian-Type Stroma: A Nationwide Multicenter Study in Japan. Pancreas, 49:181-186, 2020
2. Okamura Y, Yasukawa S, Narimatsu H, Boku N, Fukutomi A, Konishi M, Morinaga S, Toyama H, Kaneoka Y, Shimizu Y, Nakamori S, Sata N, Yamakita K, Takahashi A, Kainuma O, Hishinuma S, Yamaguchi R, Nagino M, Hirano S, Yanagisawa A, Mori K, Uesaka K. Human equilibrative nucleoside transporter-1 expression is a predictor in patients with resected pancreatic cancer treated with adjuvant S-1 chemotherapy. Cancer Sci, 111:548-560, 2020
3. Ohtsuka T, Nagakawa Y, Toyama H, Takeda Y, Maeda A, Kumamoto Y, Nakamura Y, Hashida K, Honda G, Fukuzawa K, Toyoda E, Tanabe M, Gotohda N, Matsumoto I, Ryu T, Uyama I, Kojima T, Unno M, Ichikawa D, Inoue Y, Matsukawa H, Sudo T, Takaori K, Yamaue H, Eguchi S, Tahara M, Shinzeki M, Eguchi H, Kurata M, Morimoto M, Hayashi H, Marubashi S, Inomata M, Kimura K, Amaya K, Sho M, Yoshida R, Murata A, Yoshitomi H, Hakamada K, Yasunaga M, Abe N, Hioki M, Tsuchiya M, Misawa T, Seyama Y, Noshiro H, Sakamoto E, Hasegawa K, Kawabata Y, Uchida Y, Kameyama S, Ko S, Takao T, Kitahara K, Nakahira S, Baba H, Watanabe M, Yamamoto M, Nakamura M. A multicenter prospective registration study on laparoscopic pancreatectomy in Japan: report on the assessment of 1,429 patients. J Hepatobiliary Pancreat Sci, 27:47-55, 2020
4. Shimizu Y, Mizuno S, Fujinami N, Suzuki T, Saito K, Konishi M, Takahashi S, Gotohda N, Tada T, Toyoda H, Kumada T, Miura M, Suto K, Yamaji T, Matsuda T, Endo I, Nakatsura T. Plasma and tumoral glypican-3 levels are correlated in patients with hepatitis C virus-related hepatocellular carcinoma. Cancer Sci, 111:334-342, 2020
5. Sugimoto M, Kendrick ML, Farnell MB, Nomura S, Takahashi N, Kobayashi T, Kobayashi S, Takahashi S, Konishi M, Gotohda N. Relationship between pancreatic thickness and staple height is relevant to the occurrence of pancreatic fistula after distal pancreatectomy. HPB (Oxford), 22:398-404, 2020
6. Morisue R, Kojima M, Kobayashi T, Sugimoto M, Kobayashi S, Takahashi S, Konishi M, Gotohda N. A Case Of Sarcomatoid Hepatocellular Carcinoma With Prominent PD-L1 Expression. The Internet Journal of Surgery, 36:1-7, 2020
7. Okubo S, Kojima M, Matsuda Y, Hioki M, Shimizu Y, Toyama H, Morinaga S, Gotohda N, Uesaka K, Ishii G, Mino-Kenudson M, Takahashi S. Area of residual tumor (ART) can predict prognosis after post neoadjuvant therapy resection for pancreatic ductal adenocarcinoma. Sci Rep, 9:17145, 2019
8. Martin JD, Panagi M, Wang C, Khan TT, Martin MR, Voutouri C, Toh K, Papageorgis P, Mpekris F, Polydorou C, Ishii G, Takahashi S, Gotohda N, Suzuki T, Wilhelm ME, Melo VA, Quader S, Norimatsu J, Lanning RM, Kojima M, Stuber MD, Stylianopoulos T, Kataoka K, Cabral H. Dexamethasone Increases Cisplatin-Loaded Nanocarrier Delivery and Efficacy in Metastatic Breast Cancer by Normalizing the Tumor Microenvironment. ACS Nano, 13:6396-6408, 2019
9. Sukeda A, Nakamura Y, Nishida Y, Kojima M, Gotohda N, Akimoto T, Ochiai A. Expression of Monocarboxylate Transporter 1 Is Associated With Better Prognosis and Reduced Nodal Metastasis in Pancreatic Ductal Adenocarcinoma. Pancreas, 48:1102-1110, 2019
10. Sugimoto M, Takahashi N, Farnell MB, Smyrk TC, Truty MJ, Nagorney DM, Smoot RL, Chari ST, Carter RE, Kendrick ML. Survival benefit of neoadjuvant therapy in patients with non-metastatic pancreatic ductal adenocarcinoma: A propensity matching and intention-to-treat analysis. J Surg Oncol, 120:976-984, 2019
