Annual Report 2019
Cancer Screening Center
Takahisa Matsuda, Masau Sekiguchi, Keiko Nakamura, Yasuo Kakugawa, Minori Matsumoto, Eriko Tsuruki, Masayoshi Yamada, Hiroyuki Takamaru, Takaaki Tsuchida, Masahiko Kusumoto, Gen Iinuma, Nachiko Uchiyama, Mari Kikuchi, Kimiteru Ito, Takahiro Morita, Hiroaki Kurihara, Miyuki Sone, Yasunori Mizuguchi, Hirokazu Watanabe, Mototaka Miyake, Syunsuke Sugawara, Yuko Kubo, Chihiro Ito, Nao Kikkawa, Shintaro Kimura, Sawako Kaku, Junji Omori, Mizuki Ozawa, Yuji Koretsune, Tomoyasu Kato, Mitsuya Ishikawa, Masaya Uno, Yasuhito Tanase, Mayumi Kato, Kenichi Nakamura, Hiroshi Katayama, Junko Eba, (Visiting Researcher) Ryutaro Kakinuma, Koichi Nagata, Shungo Endo, Kazutomo Togashi, Noriaki Takahashi, Takaaki Yasuda, Masaki Matsuoka, Ken Takabayashi, Hidenori Kanazawa, Shuji Yamamoto, Hidetsugu Yamagishi, Kayoko Kasuya, (Special research assistant) Mika Mori, Hiroko Shindo
Introduction
In the Cancer Screening Center (former name: Research Center for Cancer Prevention and Screening; RCCPS), we have provided opportunistic cancer screening by using newly developed modalities since 2004. Most of the staff doctors hold two positions concurrently with in both Cancer Screening Center and their own specialized department. Our Cancer Screening Center consists of 20 radiologists, eight gastroenterologists, one bronchoscopist, five gynecologists, seven radiologic technologists, five ultrasonographic technologists and four nurses. Our division is in charge of multiphasic cancer screening using several imaging modalities to develop new cancer screening systems and to assess new screening tests.
The Team and What We Do
1. Course of cancer screening: The basic plan for males consists of screening for cancer of the lung, esophagus, stomach, colorectum, liver, gall bladder, pancreas, kidney, and prostate. In the basic plan for females, the screening for cancer of the breast, uterus, and ovary are added to the plan for males, excluding the prostate. In addition, PET (positron emission tomography) is provided as an option. Other than multiphasic programs, an independent cancer screening program has been prepared for lung and female genital cancers, including cancer of the uterus and ovary, breast cancer and gastrointestinal cancer. Blood samples are also obtained for biochemistry and tumor markers such as CA19-9, CEA, CA125, PSA, and genetic analysis.
2. Eligibility criteria for participants: The cancer screening program at the Cancer Screening Center, from 2013 has been planned for applicants 40 years or older who give written informed consent for the screening, including blood samples for genetic analysis, and who take the questionnaire survey concerning lifestyles. These study protocols have been approved by the Institutional Review Board (IRB). Applicants who have been diagnosed as having cancer, and/or have a history of cancer treatment, such as surgery or endoscopic mucosal resection or chemotherapy within the previous one year, are excluded.
3. Cancer screening methods: In the multiphasic cancer screening programs (comprehensive cancer screening program), CT for lung cancer, abdominal US for cancer of the liver, gall bladder, pancreas, and kidney, gynecological examinations with pap-smear and HPV test for uterus cancer, and MMG/Tomosynthesis and US for breast cancer are performed on the first day. On the following day, gastroscopy for cancer of the esophagus and stomach, and total colonoscopy for cancer of the colon and rectum are conducted. Moreover, from the beginning of December 2010, CT-colonography (CTC) has been provided as an optional method for cancer screening. FDG-PET/CT is offered on the first day as an option, if the participants wish to undergo the examination. Furthermore, FDG-PET/MRI has been provided as an optional examination since 2018.
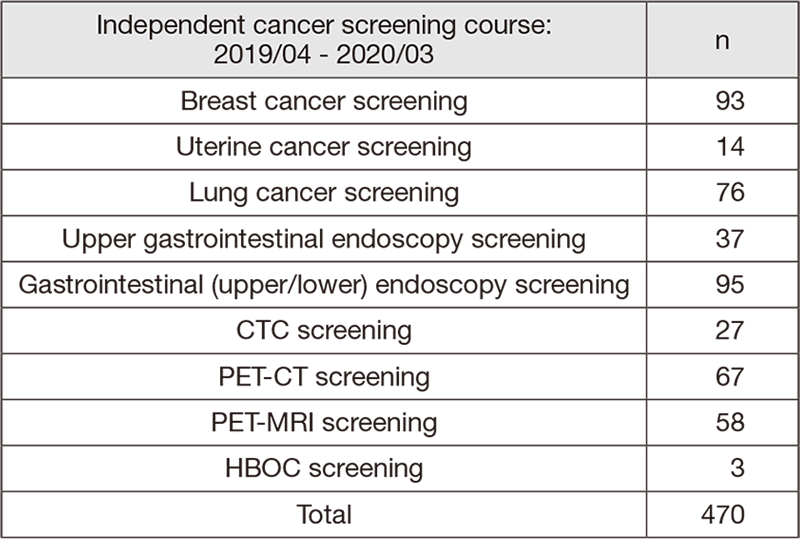
4. Number of participants of cancer screening: We present the number of participants of cancer screening between April 2019 and March 2020 in this report (Tables 1, 2). A total of 2,945 people received cancer screening at the Cancer Screening Center in this period. Most of the participants (84%; n=2,475) chose the comprehensive cancer screening course. Regarding the cancer detection rate data in each modality, we will report them in the near future.
Table 1. Number of participants in “Comprehensive cancer screening program”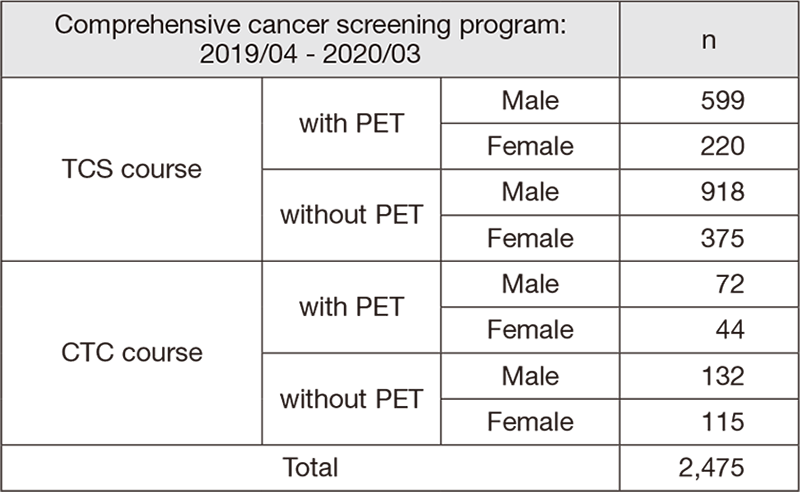
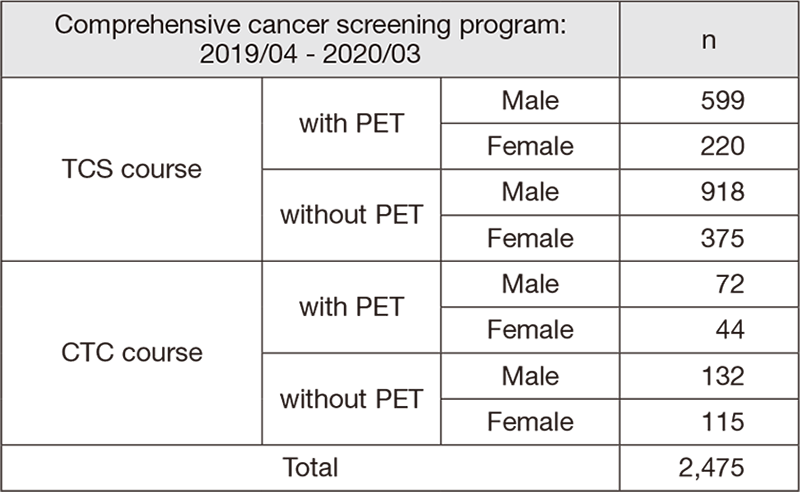
Table 2. Number of participants in “Independent cancer screening course”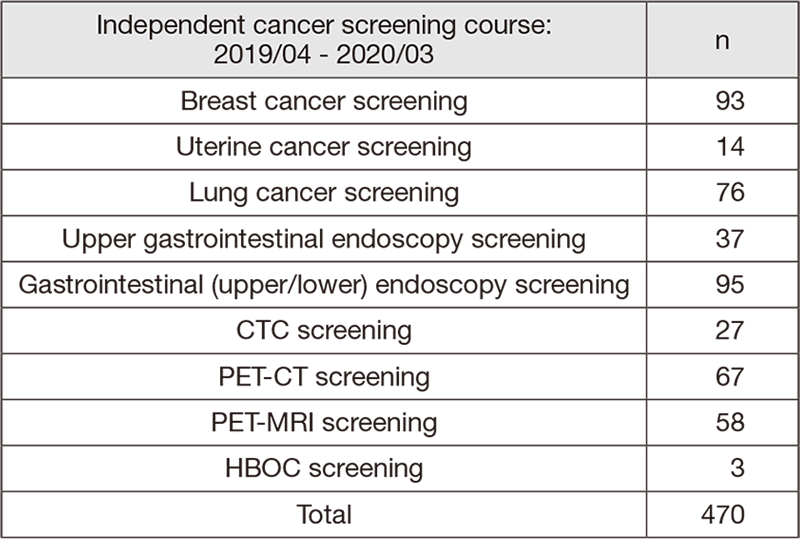
Research activities
1. Study using gastric cancer screening data from upper gastrointestinal endoscopy
We retrospectively examined the data of 15,161 first-time examinees (male: 9,165, female: 5,996, average age: 63 years) who underwent upper gastrointestinal endoscopy examination at the Cancer Screening Center. The study period was divided into 3 groups (first: 2004-2007, second: 2008-2012, third: 2013-2017), and we examined the gastric cancer detection rate and the positive rate of atrophic gastritis in each group. Although there was no difference in gender or age during each target period, the prevalence of gastric cancer and atrophic gastritis was clearly reduced over time (gastric cancer detection rate; 1.03%→0.69%→0.46%, atrophic gastritis positive rate; 72%→48%→37%).
2. Study using colorectal cancer screening data from colonoscopy (TCS)
(1) The lesion identification ability in the detailed TCS examination was analyzed using the data of the examinees who were referred to the NCCH for the purpose of colonoscopic polypectomy. It was confirmed that advanced neoplasia (ACN) of the colorectum including colorectal cancer and polyps (adenomas) of 5 mm or more can be identified with high accuracy, but the re-identification rate of diminutive polyps smaller than 5 mm is about 70%. (Sekiguchi M, et al., J Gastroenterol Hepatol 2019). (2) Analysis of the data of the examinees at the screening center revealed that only adenomas smaller than 5 mm were found in the TCS, and even if there was no follow-up treatment, the cumulative incidence of ACN over the next 5 years was as low as 1.4%. This result suggests that small colorectal adenomas may be followed up without treatment and without excessive surveillance (Sekiguchi M, et al., Am J Gastroenterol 2019).
3. Observational study of lung cancer CT screening examinees
An observational study of lung cancer CT screening examinees was conducted. The subjects were 12,114 (non-smokers, 6,021 men and 4,820 women), and 133 cases (152 lesions) of lung cancer were found. The OR of lung cancer detection in smokers over 30 pack-years is significantly higher than in nonsmokers and smokers under 30 pack-years. On the other hand, if the subjects of lung cancer CT screening in Japan are limited to smokers who smoke for 30 pack-years or more, which is the same as in the United States, about 70% of lung cancer patients may miss the opportunity to be detected by CT screening (Kakinuma R, et al., Translational Lung Cancer Research, 2020).
4. Accuracy evaluation of breast cancer screening using tomosynthesis and ABVS
The accuracy of the combined breast cancer screening was evaluated for 2,427 patients who underwent the opportunistic breast cancer screening (tomosynthesis: DBT and ABVS). Compared with the conventional method (MMG/HUS screening), the DBT/ABVS combined screening showed no significant difference, but the scrutiny rate decreased, the cancer detection rate improved, and the rate of biopsy as a scrutiny decreased. Furthermore, the positive predictive value (PPV) was significantly improved compared to the conventional MMG/HUS screening, suggesting significance of the DBT/ABVS combined screening.
5. Amino-index (AICS) cancer screening accuracy evaluation study
Since the start of the research in July 2012, we have received plasma samples from 8,111 screening examinees and are proceeding with comprehensive amino acid analysis. In the near future, we will proceed with collation work with the examination data.
Clinical trials
We are doing ongoing research work based on the study protocol titled “Evaluation of effectiveness of cancer screening modality at National Cancer Center”. The target modalities are as follows. 1) Upper gastrointestinal endoscopy, 2) Lower gastrointestinal endoscopy, 3) CT colonography, 4) Chest computed tomography (CT), 5) Sputum cytology, 6) Mammography, 7) Breast ultrasonography, 8) FDG-positron emission tomography (PET), 9) Abdominal ultrasonography, and 10) Serum tumor markers.
Future prospects
Based on cancer screening data such as examination results, medical institution findings, follow-up findings, and the questionnaire survey concerning lifestyles for 10 years, we commenced with assessment supported by the National Cancer Center Research and Development Fund.
List of papers published in 2019
Journal
1. Inoki K, Kakugawa Y, Takamaru H, Sekiguchi M, Matsumoto M, Matsuda T, Ito A, Tanaka T, Inamoto Y, Fuji S, Kurosawa S, Kim SW, Fukuda T, Ohe Y, Saito Y. Capsule Endoscopy after Hematopoietic Stem Cell Transplantation Can Predict Transplant-Related Mortality. Digestion, 101:198-207, 2020
2. Sekiguchi M, Kakugawa Y, Nakamura K, Matsumoto M, Takamaru H, Yamada M, Sakamoto T, Saito Y, Matsuda T. Feasibility of observational screening colonoscopy followed by deferred polypectomy. J Gastroenterol Hepatol, 35:263-270, 2020
3. Sekiguchi M, Kakugawa Y, Nakamura K, Matsumoto M, Tomizawa Y, Murakami Y, Saito Y, Matsuda T. Family history of colorectal cancer and prevalence of advanced colorectal neoplasia in asymptomatic screened populations in different age groups. Gastrointest Endosc, 91:1361-1370, 2020
4. Sekiguchi M, Igarashi A, Sakamoto T, Saito Y, Esaki M, Matsuda T. Cost-effectiveness analysis of colorectal cancer screening using colonoscopy, fecal immunochemical test, and risk score. J Gastroenterol Hepatol, 2020
5. Mori Y, Kudo SE, East JE, Rastogi A, Bretthauer M, Misawa M, Sekiguchi M, Matsuda T, Saito Y, Ikematsu H, Hotta K, Ohtsuka K, Kudo T, Mori K. Cost savings in colonoscopy with artificial intelligence-aided polyp diagnosis: an add-on analysis of a clinical trial (with video). Gastrointest Endosc, S0016-5107(20)34034-7, 2020
6. Abe S, Saito Y, Tanaka Y, Ego M, Yanagisawa F, Kawashima K, Takamaru H, Sekiguchi M, Yamada M, Sakamoto T, Matsuda T, Goto O, Yahagi N. A novel endoscopic hand-suturing technique for defect closure after colorectal endoscopic submucosal dissection: a pilot study. Endoscopy, 2020
7. Abe S, Wu SYS, Ego M, Takamaru H, Sekiguchi M, Yamada M, Nonaka S, Sakamoto T, Suzuki H, Yoshinaga S, Matsuda T, Oda I, Saito Y. Efficacy of Current Traction Techniques for Endoscopic Submucosal Dissection. Gut Liver, 2020
8. Katada C, Horimatsu T, Muto M, Tanaka K, Matsuda K, Fujishiro M, Saito Y, Ohtsuka K, Oda I, Kato M, Kida M, Kobayashi K, Hoteya S, Kodashima S, Matsuda T, Yamamoto H, Ryozawa S, Iwakiri R, Kutsumi H, Miyata H, Kato M, Haruma K, Fujimoto K, Uemura N, Kaminishi M, Tajiri H. Current status of esophageal endoscopy including the evaluation of smoking and alcohol consumption in Japan: an analysis based on the Japan endoscopy database. Esophagus, 16:174-179, 2019
9. Sakamoto T, Inoki K, Takamaru H, Sekiguchi M, Yamada M, Nakajima T, Matsuda T, Saito Y. Efficacy of linked colour imaging in magnifying chromoendoscopy with crystal violet staining: a pilot study. Int J Colorectal Dis, 34:1341-1344, 2019
10. Jimenez-Garcia VA, Yamada M, Ikematsu H, Takamaru H, Abe S, Sakamoto T, Nakajima T, Matsuda T, Saito Y. Endoscopic submucosal dissection in management of colorectal tumors near or involving a diverticulum: a retrospective case series. Endosc Int Open, 7:E664-E671, 2019
11. Niikura R, Yamada A, Fujishiro M, Tanaka K, Matsuda K, Saito Y, Ohtsuka K, Oda I, Katada C, Kato M, Kida M, Kobayashi K, Hoteya S, Horimatsu T, Kodashima S, Matsuda T, Muto M, Yamamoto H, Ryozawa S, Iwakiri R, Kutsumi H, Miyata H, Kato M, Haruma K, Fujimoto K, Uemura N, Kaminishi M, Shinozaki T, Tajiri H, Koike K. The Effects of Direct Oral Anticoagulants, Warfarin, Aspirin and Thienopyridine on the Performance of Immunochemical, Faecal, Occult Blood Tests. Digestion, 100:117-126, 2019
12. Kobayashi S, Yamada M, Takamaru H, Sakamoto T, Matsuda T, Sekine S, Igarashi Y, Saito Y. Diagnostic yield of the Japan NBI Expert Team (JNET) classification for endoscopic diagnosis of superficial colorectal neoplasms in a large-scale clinical practice database. United European Gastroenterol J, 7:914-923, 2019
13. Inoki K, Yamada M, Kuwabara H, Takamaru H, Sekiguchi M, Sakamoto T, Matsuda T, Saito Y. Newly-developed colonoscope (PCF-PQ260L) is useful for patients with difficult colons. Turk J Gastroenterol, 30:630-635, 2019
14. Sakamoto T, Tomizawa Y, Cho H, Takamaru H, Sekiguchi M, Yamada M, Matsuda T, Murakami Y, Saito Y. Additional value of linked color imaging in colonoscopy: a retrospective study. Endosc Int Open, 7:E1448-E1454, 2019
15. Atkinson NSS, Ket S, Bassett P, Aponte D, De Aguiar S, Gupta N, Horimatsu T, Ikematsu H, Inoue T, Kaltenbach T, Leung WK, Matsuda T, Paggi S, Radaelli F, Rastogi A, Rex DK, Sabbagh LC, Saito Y, Sano Y, Saracco GM, Saunders BP, Senore C, Soetikno R, Vemulapalli KC, Jairath V, East JE. Narrow-Band Imaging for Detection of Neoplasia at Colonoscopy: A Meta-analysis of Data From Individual Patients in Randomized Controlled Trials. Gastroenterology, 157:462-471, 2019
16. Sekiguchi M, Igarashi A, Sakamoto T, Saito Y, Esaki M, Matsuda T. Cost-effectiveness analysis of postpolypectomy colonoscopy surveillance using Japanese data. Dig Endosc, 31:40-50, 2019
17. Wong JCT, Chiu HM, Kim HS, Byeon JS, Matsuda T, Kobayashi N, Wu DC, Ong DE, Sung JJY. Adenoma detection rates in colonoscopies for positive fecal immunochemical tests versus direct screening colonoscopies. Gastrointest Endosc, 89:607-613.e1, 2019
18. Takeuchi Y, Sawaya M, Oka S, Tamai N, Kawamura T, Uraoka T, Ikematsu H, Moriyama T, Arao M, Ishikawa H, Ito Y, Matsuda T. Efficacy of autofluorescence imaging for flat neoplasm detection: a multicenter randomized controlled trial (A-FLAT trial). Gastrointest Endosc, 89:460-469, 2019
19. Sung JJY, Chiu HM, Jung KW, Jun JK, Sekiguchi M, Matsuda T, Kyaw MH. Increasing Trend in Young-Onset Colorectal Cancer in Asia: More Cancers in Men and More Rectal Cancers. Am J Gastroenterol, 114:322-329, 2019
20. Sakamoto T, Ramaraj R, Tomizawa Y, Cho H, Matsuda T, Saito Y. Clinical significance of colorectal polyp detection on colonoscopy insertion. United European Gastroenterol J, 7:125-129, 2019
21. Lee BI, Matsuda T. Estimation of Invasion Depth: The First Key to Successful Colorectal ESD. Clin Endosc, 52:100-106, 2019
22. Sekiguchi M, Otake Y, Kakugawa Y, Matsumoto M, Tomizawa Y, Saito Y, Matsuda T. Incidence of Advanced Colorectal Neoplasia in Individuals With Untreated Diminutive Colorectal Adenomas Diagnosed by Magnifying Image-Enhanced Endoscopy. Am J Gastroenterol, 114:964-973, 2019
23. Yachida S, Mizutani S, Shiroma H, Shiba S, Nakajima T, Sakamoto T, Watanabe H, Masuda K, Nishimoto Y, Kubo M, Hosoda F, Rokutan H, Matsumoto M, Takamaru H, Yamada M, Matsuda T, Iwasaki M, Yamaji T, Yachida T, Soga T, Kurokawa K, Toyoda A, Ogura Y, Hayashi T, Hatakeyama M, Nakagama H, Saito Y, Fukuda S, Shibata T, Yamada T. Metagenomic and metabolomic analyses reveal distinct stage-specific phenotypes of the gut microbiota in colorectal cancer. Nat Med, 25:968-976, 2019
24. Ichijima R, Abe S, Kobayashi S, Minagawa T, Tagawa T, Nakajima T, Yamada M, Takamaru H, Sekiguchi M, Sakamoto T, Oda I, Matsuda T, Saito Y, Gotoda T. Efficacy of Full-Spectrum Endoscopy to Visualize the Major Duodenal Papilla in Patients with Familial Adenomatous Polyposis. Digestion, 1-8, 2019
25. Inoki K, Sakamoto T, Takamaru H, Sekiguchi M, Yamada M, Matsuda T, Saito Y. The Diagnostic Performance for Colorectal Neoplasms Using Magnified Endoscopy Differs between Experts and Novice Endoscopists: A Post Hoc Analysis. Digestion, 1-8, 2019
26. Sakamoto T, Takamaru H, Sekiguchi M, Yamada M, Matsuda T, Saito Y. Reliability of Japan Narrow-Band Imaging Expert Team Classification for the Diagnosis of Colorectal Neoplasms: A Pilot Study. Digestion, 1-6, 2019
