Annual Report 2020
Department of Colorectal Surgery
Masaaki Ito, Takeshi Sasaki, Yuji Nishizawa, Yuichiro Tsukada, Koichi Teramura, Koji Ikeda, Nobuyoshi Takeshita, Hiro Hasegawa, Daichi Kitaguchi, Hiroki Kato, Yasuaki Yamamoto, Toshiyuki Adachi
Introduction
Our main purpose is to bring together the outcomes of curability and postoperative patient function with low rate of severe complications. This requires not only the establishment of effective operative techniques but also an oncological consensus, including consensus on the quality of life (QOL) and the various functions of patients with pelvic malignancies. New surgical procedures, such as two-team operation, combine the therapeutic procedures of the trans-abdominal and trans-anal approach, named trans-anal total mesorectal excision: TaTME, which can be applied to nerve-sparing surgery, sphincter-saving surgery, bladder-sparing surgery, and minimally invasive surgery. We are also establishing a methodology for providing effective preoperative treatments for advanced colorectal cancer (such as chemotherapy and chemo-radiation therapy) according to the each patient's risk factor(s) of recurrence after curative surgery.
The Team and What We Do
The Colorectal Surgery Division comprises 9 colorectal surgeons and 11 residents. The outpatient clinic is open 5 days a week. More than 400 new patients with colorectal carcinomas visited this division during the last year. Treatment plans are discussed at a weekly multidisciplinary team conference, including colorectal and hepatic surgeons, oncologists and radiologists. Many treatment strategies, such as local excision and other minimally invasive surgeries using laparoscopy, and intensive radical surgery like total pelvic exenteration, with or without adjuvant chemo- or radiotherapy, have been introduced for the treatment of patients at any stages of colorectal cancer. Laparoscopy-assisted operations with wider lymphadenectomy or combined resection of adjacent organs are also increasingly being performed for patients with advanced colorectal carcinomas. Function preserving surgery to maintain the patient's postoperative quality of life, such as intersphincteric resection, have been performed in more than 500 patients with tumors very low rectal tumors. Moreover, a strong point of our team is the extensive experience we have with the two-team TaTME rectal surgery, which starts from the perineal side and the abdominal side at the same time, contributing to shortening the operation time.
Research activities
We have published the outcomes of anus-preserving surgery for low rectal cancer, especially that of TaTME in Japan and worldwide. The results of our medical device development such as the surgical navigation system with artificial intelligence have been also published. We are proceeding with several clinical trials such as NAIR study, VOLTAGE study, JCOG1612, and JCOG1801 to improve the rectal cancer patients’ prognoses and quality of life.
Clinical trials
Phase Ib/II, multicenter study to investigate the safety, efficacy, and proof-of-concept (POC) of nivolumab monotherapy as a sequential therapy following preoperative chemoradiotherapy in patients with locally advanced resectable rectal cancer. (VOLTAGE study)
A phase III randomized controlled trial comparing surgery plus adjuvant chemotherapy with preoperative chemoradiotherapy followed by surgery plus adjuvant chemotherapy for locally recurrent rectal cancer: RC-SURVIVE study (JCOG1801)
Single-arm confirmatory trial of the adjuvant chemoradiation for the patients with the high-risk rectal submucosal invasive cancer after the local resection: RESCUE study (JCOG1612)
Oxaliplatin and fluoropyrimidine chemotherapy first vs. upfront surgery for “very low” lying locally advanced rectal cancer without preoperative chemoradiation: The NAIR phase 3 trial
Evaluation of semi-standard treatment for lower and early-staged rectal cancer (high-risk pT1, low-risk pT2) in the late elderly patients: a multicenter prospective observational study.
COLOR III Trial: Transanal vs Laparoscopic TME (COLORIII)
Education
We have guided university students in their studies, assisted colorectal surgeons in obtaining medical specialist certifications, and held a TaTME and lapaproscopic sigmoidectomy seminar for Japanese surgeons as training for surgical procedures.
Future Prospects
We aim to establish less-invasive surgery for cure and function-preservation in cancer patients with colorectal malignancies.
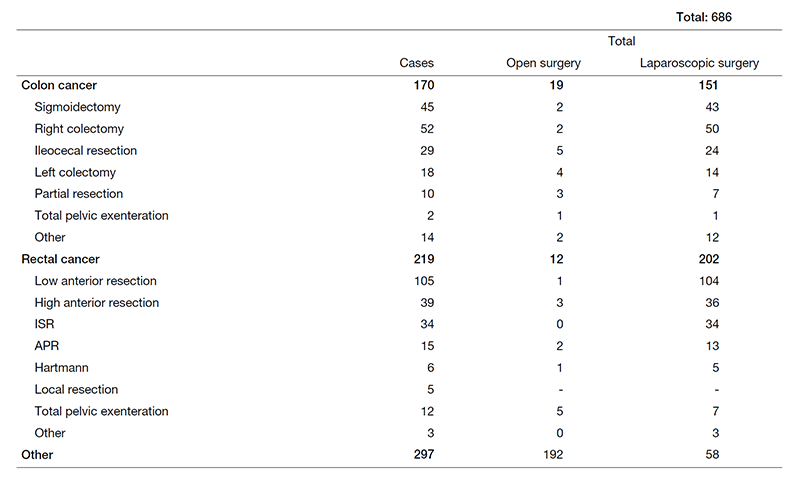
Table 1. The number of surgical cases from Apr. 2020 to Mar. 2021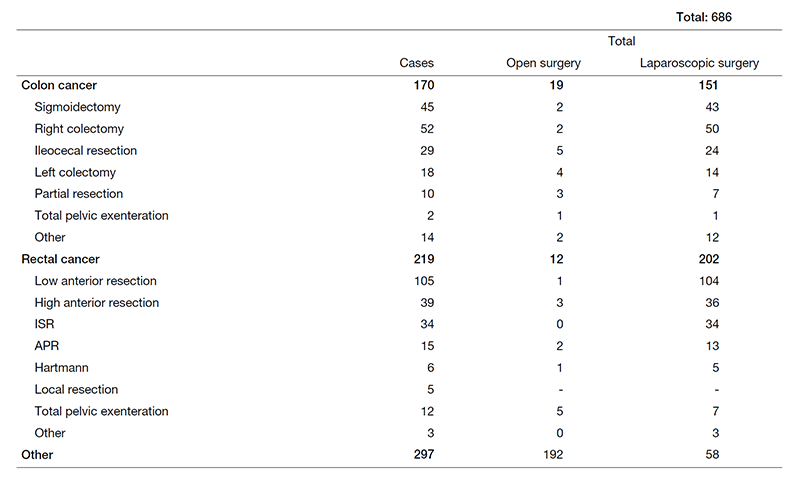
List of papers published in 2020
Journal
1. Higashino T, Sakuraba M, Fukunaga Y, Oshima A, Masuda H, Ito M. Surgical outcome for colorectal or urinary tract-related fistula: Usefulness of vascularized tissue transfer-a retrospective study(?). J Plast Reconstr Aesthet Surg, 74:1041-1049, 2021
2. Kitaguchi D, Takeshita N, Matsuzaki H, Hasegawa H, Honda R, Teramura K, Oda T, Ito M. Computer-assisted real-time automatic prostate segmentation during TaTME: a single-center feasibility study. Surg Endosc, 35:2493-2499, 2021
3. Yamaguchi T, Takahashi K, Yamada K, Bando H, Baba H, Ito M, Funahashi K, Ueno H, Fujita S, Hasegawa S, Sakai Y, Sugihara K. A nationwide, multi-institutional collaborative retrospective study of colorectal neuroendocrine tumors in Japan. Ann Gastroenterol Surg, 5:215-220, 2021
4. Narihiro S, Miura N, Nishizawa Y, Hasegawa H, Ikeda K, Teramura K, Tsukada Y, Sasaki T, Ito M. Delorme surgery for colonic mucosal prolapse after intersphincteric resection. Surg Today, 51:916-922, 2021
5. Minamide T, Ikematsu H, Murano T, Kadota T, Shinmura K, Yoda Y, Hori K, Ito M, Yano T. Metachronous advanced neoplasia after submucosal invasive colorectal cancer resection. Sci Rep, 11:1869, 2021
6. Shiraishi T, Ito M, Sasaki T, Nishizawa Y, Tsukada Y, Ikeda K. Association between urinary function and resected pattern of the autonomic nerve system after transanal total mesorectal excision for rectal cancer. Colorectal Dis, 23:405-414, 2021
7. Muro S, Tsukada Y, Ito M, Akita K. The series of smooth muscle structures in the pelvic floors of men: Dynamic coordination of smooth and skeletal muscles. Clin Anat, 34:272-282, 2021
8. Enomoto H, Nishizawa Y, Inamori K, Hasegawa H, Ikeda K, Tsukada Y, Sasaki T, Ito M. Sacral neuromodulation for the prevention of a permanent stoma in patients with severe defecation disorder following intersphincteric resection. Surg Today, 2021
9. Fukui S, Kawai T, Nishizawa Y, Nishikawa A, Nakamura T, Iwamoto N, Horise Y, Masamune K. Locally operated assistant manipulators with selectable connection system for robotically assisted laparoscopic solo surgery. Int J Comput Assist Radiol Surg, 16:683-693, 2021
10. Kondo A, Nishizawa Y, Tsukada Y, Sasaki T, Inoue M, Masuda H, Suzuki Y, Ito M. Potential benefit of laparoscopic surgery for rectal cancer on postoperative male sexual function. Colorectal Dis, 2021
11. Noguchi M, Shitara K, Kawazoe A, Yamamoto D, Takii Y, Saito Y, Sato T, Horimatsu T, Ishikawa H, Ito Y, Ito M, Ikematsu H. Short-term safety of adjuvant chemoradiotherapy after local resection for patients with high-risk submucosal invasive rectal cancer: a single-arm, multicenter phase II trial. Jpn J Clin Oncol, 51:707-712, 2021
12. Araki J, Nishizawa Y, Fujita N, Sato T, Iizuka T, Kamata M, Hatayama N, Yakura T, Hirai S, Tashiro K, Galvão FHF, Nakamura T, Nakagawa M, Naito M. Anorectal Transplantation: The First Long-Term Success in a Canine Model. Ann Surg, 2021
13. Shiraishi T, Ikeda K, Tsukada Y, Nishizawa Y, Sasaki T, Ito M, Kojima M, Ishii G, Tsumura R, Saijou S, Koga Y, Yasunaga M, Matsumura Y. High expression of TMEM180, a novel tumour marker, is associated with poor survival in stage III colorectal cancer. BMC Cancer, 21:302, 2021
14. Ouchi A, Shida D, Hamaguchi T, Takashima A, Ito Y, Ueno H, Ishiguro M, Takii Y, Ikeda S, Ohue M, Fujita S, Shiozawa M, Kataoka K, Ito M, Tsukada Y, Akagi T, Inomata M, Shimada Y, Kanemitsu Y. Challenges of improving treatment outcomes for colorectal and anal cancers in Japan: the Colorectal Cancer Study Group (CCSG) of the Japan Clinical Oncology Group (JCOG). Jpn J Clin Oncol, 50:368-378, 2020
15. Ito M, Yamamoto S, Okuda J, Fujii S, Yamaguchi S, Otsuka K, Yoshimura K, Watanabe M. Long-term survival outcomes following laparoscopic surgery for clinical stage 0/I rectal carcinoma. Ann Gastroenterol Surg, 4:294-300, 2020
16. Shiraishi T, Nishizawa Y, Ikeda K, Tsukada Y, Sasaki T, Ito M. Risk factors for parastomal hernia of loop stoma and relationships with other stoma complications in laparoscopic surgery era. BMC Surg, 20:141, 2020
17. Kitaguchi D, Takeshita N, Matsuzaki H, Oda T, Watanabe M, Mori K, Kobayashi E, Ito M. Automated laparoscopic colorectal surgery workflow recognition using artificial intelligence: Experimental research. Int J Surg, 79:88-94, 2020
18. Takahashi H, Hamabe A, Hata T, Nishizawa Y, Nishimura A, Itoh M, Takemasa I. Prospective multicenter study of reduced port surgery combined with transvaginal specimen extraction for colorectal cancer resection. Surg Today, 50:734-742, 2020
19. Imaizumi K, Nishizawa Y, Ikeda K, Tsukada Y, Sasaki T, Ito M. Prognostic Impact of Curative Resection for Peritoneal Recurrence of Colorectal Cancer. Ann Surg Oncol, 27:2487-2497, 2020
20. Kadota T, Ikematsu H, Sasaki T, Saito Y, Ito M, Mizutani T, Ogawa G, Shitara K, Ito Y, Kushima R, Kanemitsu Y, Muto M. Protocol for a single-arm confirmatory trial of adjuvant chemoradiation for patients with high-risk rectal submucosal invasive cancer after local resection: Japan Clinical Oncology Group Study JCOG1612 (RESCUE study). BMJ Open, 10:e034947, 2020
21. Nakagawa H, Tanaka K, Sasai H, Nishizawa Y. Providing Weight Loss Support to Patients Who Are Obese in Preparation for Colorectal Cancer Surgery to Reduce Surgical Site Infection Risk: A Mixed-methods Study. Wound Manag Prev, 66:23-32, 2020
22. Kadota T, Tsukada Y, Ito M, Katayama H, Mizusawa J, Nakamura N, Ito Y, Bando H, Ando M, Onaya H, Fukuda H, Kanemitsu Y. A phase III randomized controlled trial comparing surgery plus adjuvant chemotherapy with preoperative chemoradiotherapy followed by surgery plus adjuvant chemotherapy for locally recurrent rectal cancer: Japan Clinical Oncology Group study JCOG1801 (RC-SURVIVE study). Jpn J Clin Oncol, 50:953-957, 2020
23. Kitaguchi D, Takeshita N, Matsuzaki H, Takano H, Owada Y, Enomoto T, Oda T, Miura H, Yamanashi T, Watanabe M, Sato D, Sugomori Y, Hara S, Ito M. Real-time automatic surgical phase recognition in laparoscopic sigmoidectomy using the convolutional neural network-based deep learning approach. Surg Endosc, 34:4924-4931, 2020
24. Imai S, Ito M. A novel surgical training simulator for transanal total mesorectal excision. Tech Coloproctol, 24:1163-1168, 2020
25. Inoue A, Murata K, Komori T, Takeda T, Fujii M, Yamaguchi T, Yamaguchi T, Masuishi T, Shiota T, Morita S, Suzuki Y, Ito M, Kanemitsu Y, Shiozawa M, Yasui M, Kagawa Y, Sugihara K. Open versus laparoscopic surgery for primary appendiceal tumors: a large multicenter retrospective propensity score-matched cohort study in Japan. Surg Endosc, 2020
26. Ito M. ISR for T1-2 Low Rectal Cancer: A Japanese Approach. Clin Colon Rectal Surg, 33:361-365, 2020
27. Fung TLD, Tsukada Y, Ito M. Essential anatomy for total mesorectal excision and lateral lymph node dissection, in both trans-abdominal and trans-anal perspective. Surgeon, 2020
Book
1. Ito M. Robotic Surgery: Currently and in the Near Future. In: Takenoshita S, Yasuhara H (eds), Surgery and Operating Room Innovation, Singapore, Springer Singapore, pp 125-131, 2021
