Annual Report 2020
Department of Anesthesiology
Hiroyuki Yamamoto, Manabu Hashimoto, Aiko Ohshita, Reiko Sato, Kazuaki Hiraga
Introduction
In 2017, the Center for Developing Next-generation Endoscopic-surgical Treatment (NEXT) was completed to expand surgical and endoscopic activities. The operating theater which has twelve operating rooms is located on the fourth floor of the NEXT building. Each room is designed for laparoscopic, thoracoscopic and other minimally invasive surgeries. The intensive care unit (ICU) on the third floor has eight beds. Postoperative patients can be transferred from the operating theater by elevator directly to the ICU. Recently, complex procedures have been increasingly employed on more seriously ill patients with coronary disease, chronic obstructive pulmonary disease (COPD), neurological disorders, etc. In the post-anesthesia care for these patients, the ICU plays an important role. We therefore manage the operating theater in close cooperation with the Department of Intensive Care Medicine. The goals of the Department of Anesthesiology are to provide anesthetic care to patients, with their safety being the highest priority.
The Team and What We Do
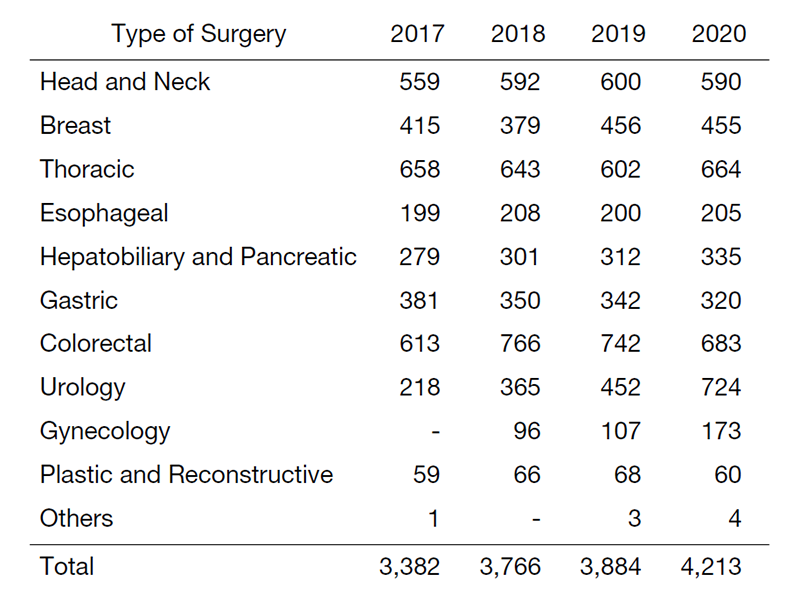
The Department of Anesthesiology consists of five staff members (four Fellows of JSA and a JSA Board Certified Anesthesiologist). We perform clinical work with two or three rotating residents and 15 part-time anesthesiologists. In addition, anesthesia residents who belong to the anesthesia training program of Teikyo University started to rotate to our department in 2018. A pre-anesthesia case presentation is held every morning to examine the cases of the day and discuss the anesthesia issues and strategies for patients with various complications. In the old operating theater which had eight operating rooms, more than 3,000 surgeries were performed every year (Table 1). With the increase in the number of operating rooms, the annual operation volume reached 3,700 this year. The large number of operations in the head and neck surgery division and procedures involving thoracotomy for lung and esophageal cancer surgeries are the features of this hospital. Accordingly, a special anesthesia induction method for difficult airways and the one-lung ventilation technique for thoracotomy are often necessary.
Education
Our department has no residents. For rotating residents from other surgical divisions, we provide opportunities for applying epidural anesthesia, one-lung ventilation technique for thoracotomy, and difficult airway management including fiberoptic intubation. This experience is useful for managing postoperative patients in the ward and ICU. A Journal Club is also held once a week in addition to the daily morning conference. We support residents who seek to obtain the qualification of Registered Anesthesiologist or JSA Qualified Anesthesiologist during rotation periods.
Future Prospects
We increased the number of operating rooms for anesthesia services from eight to nine in FY2019. In FY2020, we performed more than 4,000 surgeries. We aim for safer and higher quality management.
