Annual Report 2020
Department of Esophageal Surgery
Hiroyuki Daiko, Junya Oguma, Koshiro Ishiyama, Daisuke Kurita, Kyohei Kanematsu, Kentaro Kubo, Yusuke Fujii, Daichi Utsunomiya
Introduction
The Department of Esophageal Surgery deals with neoplasms arising from the esophagus. The surgical management of esophageal cancer has been the main clinical research activity of this department. In particular, our department is striving to establish minimally invasive surgery that consists of neoadjuvant treatment followed by minimally invasive esophagectomy. Our department is conducting a study to define the role of surgery in the multimodal approach to the treatment of esophageal cancer, and is aiming for thoracolaparoscopic esophagectomy, which consists of thoracoscopic esophagectomy and laparoscopic reconstruction, to become a standard surgical procedure. Moreover, robotic esophagectomy and gastric reconstruction were introduced in 2018.
The Team and What We Do
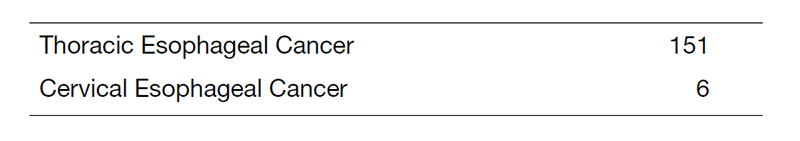
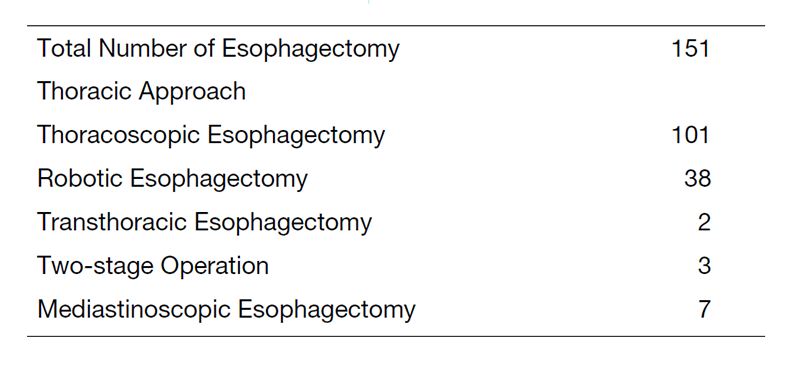
The Department of Esophageal Surgery consists of three staff surgeons and five residents. An Esophageal Conference is held every Wednesday evening to discuss the diagnosis, staging, and treatment strategy for each patient and is attended by surgeons, medical oncologists, endoscopists, radiologists, radiation oncologists, and head & neck surgeons. Approximately four patients are operated upon every week. In 2020, 157 patients underwent esophagectomies, including 151 cases of thoracic esophageal cancer and 6 cases of cervical cancer. Transthoracic esophagectomies with extended lymph node dissection were performed on 2 cases. Thoracoscopic esophagectomies in the prone position with radical lymph node dissection were undertaken in 101 cases. Bilateral transcervical mediastinoscopic laparoscopic-assisted esophagectomy for patients above 80 or patients with multiple complications was undertaken in 7 cases. Postoperatively, within 30 days, no patients died after esophagectomy.
Research Activities
Currently, our department is examining the role of thoracolaparoscopic esophagectomy as a minimally invasive esophagectomy that consists of thoracoscopic esophagectomy and laparoscopic reconstruction. For patients without radical chemoradiotherapy, thoracoscopic esophagectomy in the prone position with radical lymph node dissection and laparoscopic reconstruction after esophagectomy for patients without a history of laparotomy are being attempted to make them a standard surgical procedure for esophageal cancer.
For treating patients aged over 80 years or at high risk, a two-stage surgical procedure divided into resection and reconstruction is being attempted.
A Phase III study of tri-modality combination therapy with induction docetaxel, cisplatin, 5-fluorouracil (DCF) vs definitive chemoradiotherapy (dCRT) for locally advanced unresectable squamous cell carcinoma of the thoracic esophagus (JCOG1510, TRIANgLE trial) is ongoing.
A randomized controlled phase III study of minimally invasive versus open esophagectomy for thoracic esophageal cancer (JCOG1409, MONET trial) is ongoing.
A feasibility study of nivolumab as neoadjuvant chemotherapy for locally esophageal carcinoma (JCOG1804E, FRONTiER) is ongoing.
Since 2000, our department has been performing salvage surgery for patients in whom definitive chemoradiotherapy has failed. The operative procedures and postoperative management have been refined gradually. Our department is also studying the role and efficacy of salvage surgery in the multimodal treatment of esophageal cancer.
List of papers published in 2020
Journal
1. Nomura H, Hatogai K, Maki Y, Mochizuki N, Tanaka M, Saito S, Daiko H, Kojima T, Kawasaki T. Risk factors for febrile neutropenia in neoadjuvant docetaxel,cisplatin, and 5-fluorouracil chemotherapy for esophageal cancer. Support Care Cancer. 2020: 28(4):1849-1854
2. Takashima K, Fujii S, Komatsuzaki R, Komatsu M, Takahashi M, Kojima T, Daiko H, Minashi K, Chiwaki F, Muto M, Sasaki H, Yano T. CD24 and CK4 are upregulated by SIM2, and are predictive biomarkers for chemoradiotherapy and surgery in esophageal cancer. Int J Oncol. 2020: 56(3):835-847
3. Sakaki A, Kanamori J, Ishiyama K, Kurita D, Oguma J, Daiko H.
Distribution of lymph node metastases in locally advanced adenocarcinomas of the esophagogastric junction (cT2-4): Comparison between Siewert-type I and selected Siewert-type II tumors. Langenbeck's Archives of Surgery. 2020: 405(4):509-519
4. Daiko H, Kato K. Updates in the 8th Edition of the TNM Staging System for Esophagus and Esophagogastric Junction Cancer. Jpn J Clin Oncol. 2020: 4;50(8):847-851
5. Nomura H, Tsuji D, Demachi K, Mochizuki N, Matsuzawa H, Yano T, Daiko H, Fujii S, Kojima T, Itoh K, Kawasaki T. ABCB1 and ABCC2 genetic polymorphism as risk factors for neutropenia in esophageal cancer patients treated with docetaxel, cisplatin, and 5-fluorouracil chemotherapy. Cancer Chemother Pharmacol. 2020: 86(2):315-324
6. Kurita D, Oguma J, Ishiyama K, Hirano Y, Kanamori J, Daiko H. Handgrip Strength Predicts Postoperative Pneumonia After Thoracoscopic-Laparoscopic Esophagectomy for Patients With Esophageal Cancer. Ann Surg Oncol. 2020: 27(9):3173-3181
7. Okada N, Fujita T, Kanamori J, Sato A, Kurita D, Horikiri Y, Sato T, Fujiwara H, Yamamoto H, Daiko H. Efficacy of prewarming prophylaxis method for intraoperative hypothermia during thoracoscopic esophagectomy. Esophagus. 2020: 17(4):385-391
8. Daiko H, Marafioti T, Fujiwara T, Shirakawa Y, Nakatsura T, Kato K, Puccio I, Hikichi T, Yoshimura S, Nakagawa T, Furukawa M, Stoeber K, Nagira M, Ide N, Kojima T. Exploratory open-label clinical study to determine the S-588410 cancer peptide vaccine-induced tumor-infiltrating lymphocytes and changes in the tumor microenvironment in esophageal cancer patients. Cancer Immunology. 2020: 69(11):2247-2257
9. Hirano Y, Fujita T, Sato K, Kurita D, Sato T, Ishiyama K, Fujiwara H, Oguma J, Daiko H.Totally Mechanical Collard Technique for Cervical Esophagogastric Anastomosis Reduces Stricture Formation Compared with Circular Stapled Anastomosis. World J Surg. 2020: 44(12):4175-4183
10. Leng XF, Daiko H, Han YT, Mao YS. Optimal preoperative neoadjuvant therapy for resectable locally advanced esophageal squamous cell carcinoma. Ann N Y Acad Sci. 2020: 1482(1):213-224
11. Wang Z, Mao Y, Gao S, Li Y, Tan L, Daiko H, Liu S, Chen C, Koyanagi K, He J. Lymph node dissection and recurrent laryngeal nerve protection in minimally invasive esophagectomy. Ann N Y Acad Sci. 2020: 1481(1):20-29
12. Bin Li, Yang Y, Toker A, Yu B, Kang CH, Abbas G, Soukiasian HJ, Li H, Daiko H, Jiang H, Fu J, Yi J, Kernstine K, Migliore M, Bouvet M, Ricciardi S, Chao YK, Kim YH, Wang Y, Yu Z, Abbas AE, Sarkaria IS, Li Z; International consensus statement on robot-assisted minimally invasive esophagectomy (RAMIE). J Thorac Dis. 2020: 12(12):7387-7401
13. Yachida T, Oda I, Abe S, Sekiguchi M, Nonaka S, Suzuki H, Yoshinaga S, Taniguchi H, Sekine S, Masugata H, Masaki T, Daiko H, Saito Y. Risk of Lymph Node Metastasis in Patients with the Superficial Spreading Type of Esophageal Squamous Cell Carcinoma. Digestion. 2020: 101(3):239-244
14. Hara H, Mizusawa J, Hironaka S, Kato K, Daiko H, Abe T, Nakamura K, Ando N, Kitagawa Y. Influence of Preoperative Chemotherapy-Induced Leukopenia on Survival in Patients With Esophageal Squamous Cell Carcinoma: Exploratory Analysis of JCOG9907. Esophagus. 2021; 18(1):41-48
15. Wada S, Sadahiro R, Matsuoka YJ, Uchitomi Y, Yamaguchi T, Sato T, Shimada K, Yoshimoto S, Daiko H, Kanemitsu Y, Kawai A, Kato T, Fujimoto H, Shimizu K. Yokukansan for Treatment of Preoperative Anxiety and Prevention of Postoperative Delirium in Cancer Patients Undergoing Highly Invasive Surgery. J-SUPPORT 1605 (ProD Study): A Randomized, Double-Blind, Placebo-Controlled Trial. J Pain Symptom Manage. 2021; 61(1):71-80
16. Kanamori J, Abe S, Kurita D, Ishiyama K, Hirano Y, Oguma J, Oda I, Saito Y, Daiko H. Minimally invasive hybrid surgery: A salvage tumor enucleation for local recurrence of thoracic esophageal carcinoma after definitive chemoradiotherapy. Asian J Endosc Surg. 2021; 14(1):77-80
