Annual Report 2021
Department of Radiological Technology
I. Radiological Diagnosis
Tomohiko Aso, Shoichi Katsuta, Kanyu Ihara, Toshihiro Ishihara, Hirobumi Nagasawa, Chieko Nagashima, Toshimitsu Utsuno, Naoya Ikeno, Yoshiaki Miyazaki, Hiromi Suzuki, Atsushi Shishido, Makoto Mimatsu, Jun Torii, Yasutake Ishikawa, Minami Maruyama, Ryo Kikuchi, Hiroki Miyazaki, Eiko Taguchi, Yusuke Miyamoto, Yuya Kanai, Ryo Kawana, Yusuke Wakatsuki, Ikuya Ishii, Yuto Tanaka, Xiao Ang Tang, Seiya Mochizuki, Yuhei Shimizu, Seiya Sato, Yuta Miyamae, Akira Yoshida, Masae Fujisawa, Aya Shimoike, Shogo Nakamura, Miku Kousaka, Chihiro Muto, Chihiro Kuroki, Ken Shimizu, Satsuki Watanabe, Kazuki Matsubara, Ai Arisue, Takumi Miyairi, Ayame Sugo, Tomoka Harada, Kouki Fukushi, Yutaro Tsukahara, Yusuke Taira, Yuki Hirayama, Yoshiki Ishihara, Sayaka Shimoda, Kaho Miyagi, Ryo Hosono, Yuki Tsunoda, Yuka Kondo, Kanako Matsuda
Introduction
Diagnostic radiology devices are essential for diagnosis, staging, response to treatment, and follow-up of cancer patients. The Department of Radiological Technology makes full use of the latest technology to provide precise medical images for patients. Human resource development of radiological technologists has always been a theme in our department and continues to be. We accept and educate residents in radiological technology. Further, we have accepted students and trainees of radiological technology from all over the world for global human resource development, but the COVID-19 pandemic prevented this during FY2021.
Table 1. Number of diagnostic imaging devices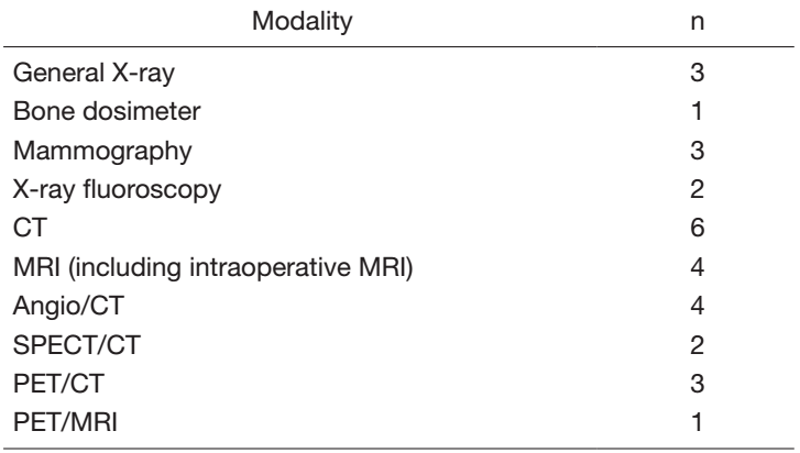
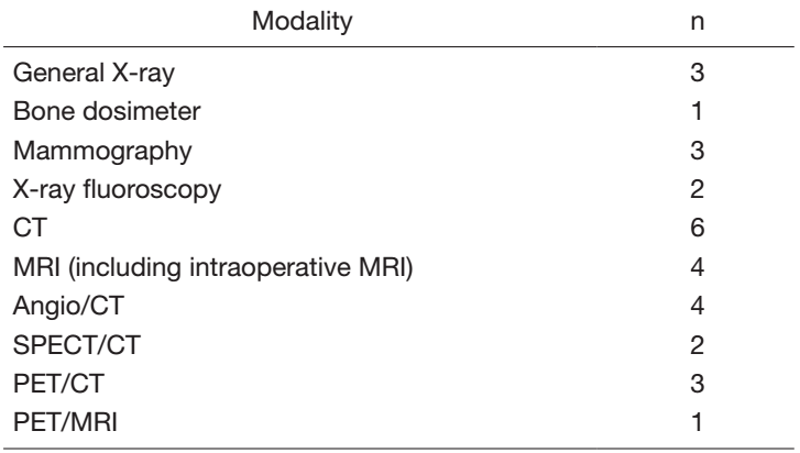
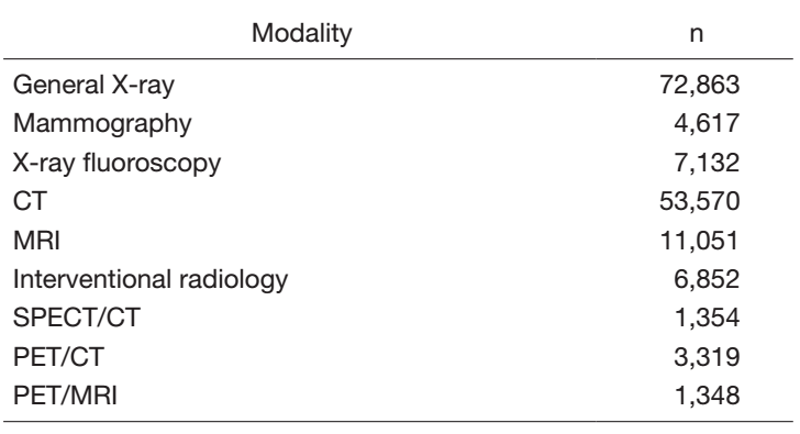
Table 2. Number of examination cases in FY2021 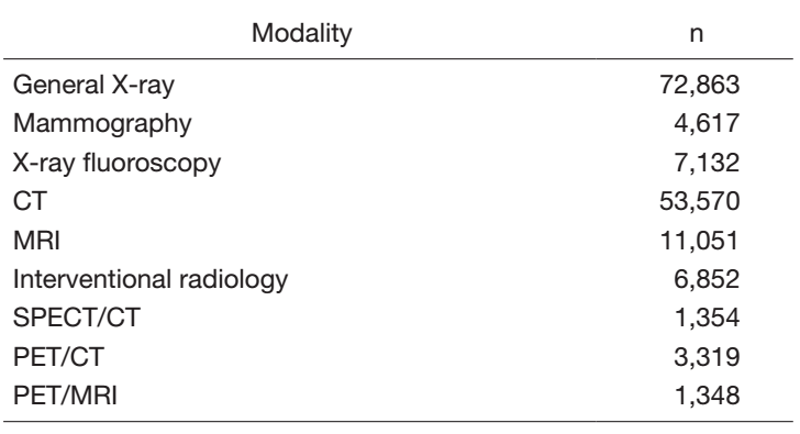
The Team and What We Do
The National Cancer Center Hospital has diagnostic imaging devices as shown in Table 1. We performed a total of 162,106 examinations as shown in Table 2 while in the COVID-19 crisis in FY2021.
The general radiography team conducted a collaborative study using an alcohol-based silver ionic agent as one of the infection prevention measures. The silver ionic agents were effective in infection control everywhere, including floating tables, chest stands, operator consoles, changing rooms, and their doorknobs.
The mammography team performed a detailed test for quality control by using a semiconductor multifunctional X-ray dosimeter.
The computed tomography (CT) team provided various additional information for diagnostic imaging using techniques such as deep learning-based reconstruction, iodine maps, and virtual monochromatic energy imaging. They conducted joint research with companies on dual energy and high-definition imaging, as well as a collation system using IC tags attached to syringes of contrast medium.
The magnetic resonance imaging (MRI) team has prepared an operations and procedures manual to equalize the number of examination cases between each scanner and has also optimized the use of contrast media.
The interventional radiology team implemented close interprofessional information sharing to provide high-quality team care and has worked on creating and processing various 3-dimensional images for pre-interventional simulation to support diagnosis and treatment. In addition, novel applications were being developed in collaboration with some companies.
The gastrointestinal radiography team has engaged in comprehensive gastrointestinal examinations, performing contrast-enhanced gastrointestinal tract examinations and CT-colonography using X-TV and X-ray CT, respectively. Further, a specialized team has been available for chest CT and chest X-ray examinations for COVID-19 patients.
The endoscopic radiography team constructed and optimized scanning parameters by applying a deep learning-based reconstruction to support CT-guided bronchoscopy using ultra-high resolution CT.
The nuclear medicine team has filed legal proceedings for the renewal of two positron emission tomography (PET)/CT systems, one of which was completed and installed by the end of FY2021. Novel internal radiation therapy for neuroendocrine tumors (peptide receptor radionuclide therapy) was initiated. They conducted joint research on an automatic combined dispenser and injector system and reported the results of their research on networking and simplification of dose management and dose information record acquisition.
Research activities
We conducted research in the fields of digital radiography (DR), CT, interventional radiology, and PET and presented the results at intra- and international conferences. We also conducted joint research with relevant companies as below.
A study comparing DR and CT was conducted to assess the detectability of dynamic imaging of abnormal lung shadows. A study on the diagnosis of malignancies using ultra-high resolution CT was performed by means of physical and clinical analysis. Further, physical image data were analyzed for studies on the diagnosis of malignancies using dual-energy CT. We performed a phantom study to analyze the physical image characteristics of deep learning-based image processing software developed for reducing image noise in CT. We also studied the use of dose management software to build a system that discloses and shares the medical exposure dose to/with patients. In the field of nuclear medicine, we performed a study of dose recording and administration using an automated dosimetry system for 18F-fluorodeoxyglucose (18F-FDG) PET examinations which resulted in a significant reduction in work time and improved efficiency due to the use of QR codes to manage commercially supplied 18F-FDG drugs.
Education
- Younger technologists participated in the training seminars hosted by the Ministry of Health, Labour and Welfare, the National Hospital Organization, and others; however, due to the COVID-19 pandemic, almost all of the seminars were conducted online.
- At the conference within the Department of Radiology Diagnostic Technology, senior technologists shared their specialized knowledge and contributed to improving skills.
- We have been conducting ongoing multi-site videoconferences with cancer hub hospitals in Japan. Even during the COVID-19 pandemic, this was effective for sharing information on radiological technology between institutes.
- We accepted hospital internship students from Juntendo University, the International University of Health and Welfare, Tokyo Metropolitan University, Kyorin University, Komazawa University, and Tsukuba International University.
- We conducted personnel exchanges with Tokyo University Hospital and Kyoto University Hospital to provide mutually enriching education.
Future Prospects
The Department of Radiological Technology has established a residency program for radiological technologists, which will begin accepting residents in FY2022 and will provide continuing education to technologists specializing in cancer medicine.
II. Radiological Oncology
Tomohiko Aso, Shouichi Katsuta, Tomonori Goka, Ako Aikawa, Toshimitsu Sofue, Miyuki Murata, Yosihiro Shibata, Watanabe Yuusuke, Tatsuya Sakasai, Yuuki Miura, Rie Ishikawa, Yuuya Hisaki, Mitsuhiro Kon, Daisuke Fujiyama, Junichi Kuwahara, Seiya Satou, Shimoike Aya, Shutou Yasunori, Miku Kousaka, Hironori Murakami, Nonaka Midori, Kazuki Takasou, Ueda Masataka, Kasai Yuusaku, Hata Ruka, Hanzawa Takuma, Hiroko Sugaya
Introduction
The Radiological Oncology unit in Department of Radiological Technology is home to four linear accelerators, a CyberKnife, an MRI-guided radiotherapy system (MRIdian), and image-guided radiation therapy (IGRT) and image-guided brachytherapy (IGBT) systems, which we use to provide various radiotherapy treatments, including intensity modulated radiation therapy (IMRT), stereotactic radiation therapy (SRT), and high-dose-rate brachytherapy with IGBT.
The Team and What We Do
1) The body stereotactic irradiation cases increased and we performed 163 cases using two high-precision positioning support systems (ExacTrac).
2) Radiotherapy applied with the MRIdian system was performed in 45 cases. Further, a total of 83 sessions of online adaptive treatment, which is a state-of-the-art of radiation therapy technique, were performed. In addition, the original cobalt MRIdian system has upgraded to a linear accelerator system in November 2021, with the aim of restarting treatment in FY2022.
3) A total of 181 cases were performed with stereotactic irradiation using a CyberKnife, consisting of 171 head-and-neck region and 10 trunk cases.
4) Total-body irradiation for bone marrow transplantation was performed in 48 cases.
5) Interstitial brachytherapy using a 106-Ru source and intertissue irradiation using a 198-Au source were performed in 20 and 2 cases, respectively. High-dose-rate intracavitary brachytherapy increased due to the use of image-guided brachytherapy treatment and was performed in 216 cases of interstitial and intracavitary brachytherapy (hybrid brachytherapy).
6) To prevent COVID-19, we reinforced infection precautions and managed the business continuity plan.
Research activities
We have developed a video display system for the respiratory motion management of patients during radiation treatment with the MRIdian system.
Clinical trials
1) A clinical study of brachytherapy using alpha particle emitting radioisotopes below the lower limit of the regulations was conducted for two patients.
2) We completed a Phase I clinical trial of boron neutron capture therapy (BNCT) performed on four patients.
Education
1) We had job rotations among modalities corresponding to our educational programs.
2) One of the radiological technologists belonging to the radiotherapy team was concurrently appointed to the Section of Radiation Safety and Quality Assurance to learn about radiotherapy planning and quality control.
3) We reviewed and improved our workflow through comprehensive training about the processes of radiotherapy.
4) We performed review and organization of the curriculum of the residency program for radiological technologists with specialized knowledge and skills, which will begin accepting residents in FY2022.
Future Prospects
1) We will continue to work together to complete the clinical trials in BNCT and achieve early clinical use.
2) We will establish an efficient quality control system and education system to contribute to spreading safe use of the MRIdian radiotherapy system.
3) To achieve advanced radiotherapy in the future, we will change the MRIdian system’s radiation source from 60-cobalt to a linear accelerator in early FY2022.
4) RALS will be replaced and updated to a high-dose-rate system, which will enable safe treatment and increase accurate outcomes.
5) The linear accelerator we have had for over 10 years will be replaced with a higher-precision one, and adaptive radiotherapy will be planned to provide stable and precise treatment.
6) We will continue to cooperate with the clinical trials performed in the Department of Radiation Oncology.
