Annual Report 2022
Department of Psycho-Oncology
Full-time staff psycho-oncologist: Hiromichi Matsuoka, Rika Nakahara, Takatoshi Hirayama, Ryoichi Sadahiro, Yosuke Uchitomi, Asako Mitsutake
Full-time staff psychologist: Yuko Yanai, Yuko Ogawa, Ayako Kayano
Part-time staff psycho-oncologist: Saho Wada
Part-time staff psychologist: Yuki Mashiko, Kyoka Ogata, Sayaka Jinno, Kazuko Matsumoto
Introduction
The Department of Psycho-Oncology was reestablished in September 1995, together with the establishment of the Psycho-Oncology Division, National Cancer Center Research Institute East (reorganized to Division of Psycho-Oncology, Research Center for Innovative Oncology in 2005). One of the most important clinical activities of the department is the management of cancer patients’ behavioral and social problems as well as their psychological distress. Furthermore, this division’s aim is to alleviate the distress of patients, patients’ families and our staff. Our research activity is focused on studying the psychosocial influence of cancer on the quality of life of patients, their families, and oncology staff.
The Team and What We Do
The Department of Psycho-Oncology consists of six full-time staff psycho-oncologists, one part-time psychiatrist, three full-time staff psychotherapists and four part-time psychotherapists. The department provides two major services: a clinic for outpatients (five days a week) and consultation for referred inpatients. The purpose of the psychiatric consultation is to diagnose and treat the mental distress and cancer-related psychological problems of patients who have been referred by their attending physicians. Since 1999, the department has played an active role as a member of the palliative care team. There is a palliative care team meeting with other members of the team every Tuesday. Additionally, a multicenter joint clinical teleconference to discuss difficult cases is held biweekly on Thursday evenings with staff members from 6 cancer center hospitals and 4 university hospitals.
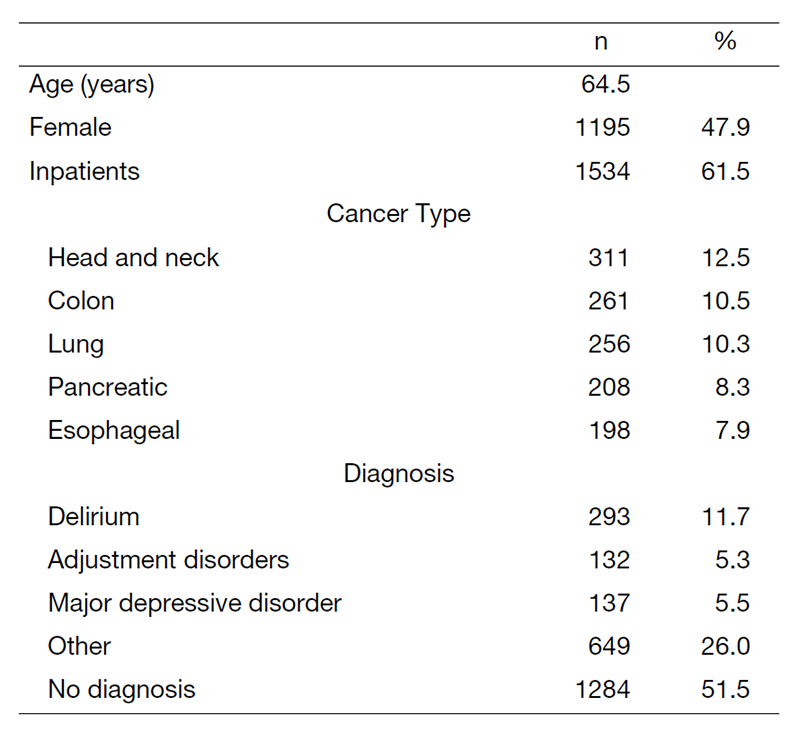
In 2022, a total of 2495 patients were referred for psychiatric consultation (Table 1). The mean age was 64.5 years, and 61.5% of the referrals were inpatients. Females accounted for 1195 cases (47.9%) of the whole referred patients (Table 1). The most common cancer referrals were patients with head and neck cancer (12.5%), followed by colon cancer (10.5%), lung cancer (10.3%), pancreatic cancer (8.3%) and esophageal cancer (7.9%).
The most common psychiatric diagnosis which is based on the DSM-5 criteria (Diagnostic and Statistical Manual of Mental Disorders, 5th edition) was delirium (11.7%), followed by major depressive disorder (5.5%) and adjustment disorders (5.3%), while 51.5% of the referrals had no psychiatric diagnosis. Three common mental disorders (delirium, adjustment disorders, and major depressive disorder) were responsible for half of the psychological problems.
Table 1. Psychiatric Consultation Data in 2022 (n=2495)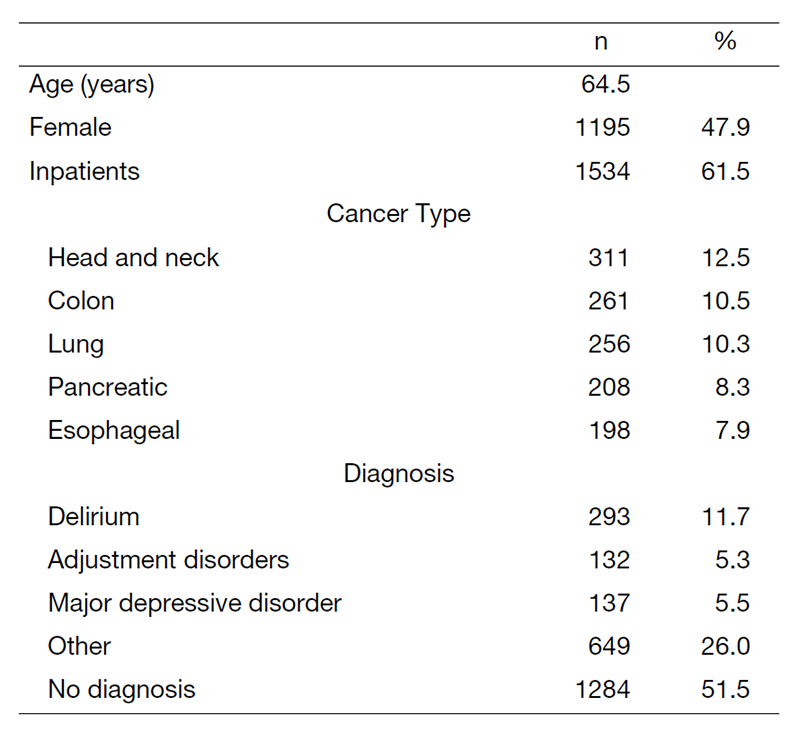
Research Activities
In collaboration with the Department of Hematopoietic Stem Cell Transplantation, we are planning to develop a psychological support program for allogeneic hematopoietic stem cell transplantation ("transplant") survivors. This year, we are publishing a retrospective study at our center using pre-transplant assessment and medical records of patients who have used psycho-psychological support, with the aim of identifying psychological issues (e.g., psychological characteristics and support needs) among allogeneic transplant patients.
A semi-structured interview survey of 40 AYA cancer patients at our hospital was conducted, and a screening tool for determining distress and supportive care needs of AYA cancer patients in Japan was developed based on the Distress Thermometer and Problem List of the NCCN®. We have suggested the feasibility, validity, and reliability of the screening tool, and published a paper on the results. Furthermore, a psychosocial support program using the screening tool was developed, and a multicenter observational study was conducted at 8 institutions in Japan. The feasibility and effectiveness of the program were suggested, and the results are currently being published.
Clinical Trials
We planned advanced medical care, a clinical trial with the aim of adding prevention of delirium to the insurance indication for ramelteon, which was deemed suitable. Plans were also made to develop biomarkers to predict the efficacy of ramelteon and the onset of delirium, and a new AMED research grant was obtained. In addition, as a companion study to the clinical trial to prevent delirium using yokukansan, a biomarker to predict the efficacy of yokukansan is being developed with Tsumura Corporation under the support of the AMED.
Education
We are working to develop educational programs for psycho-oncologists, pharmacists, nurses, and psychologists. In the future, we intend to establish a training system that enables doctors, psychotherapists, and other professionals involved in psychiatric oncology to learn systematically and contribute to the improvement of the quality of life of cancer patients in Japan by producing specialists in psychiatric oncology throughout the country.
Future Prospects
We are now developing an ideal system of early palliative care for all cancer patients.
List of papers published in 2022
Journal
1. Hirayama T, Ikezawa S, Okubo R, Mizuta T, Iwata S, Suzuki T. Mental health care use and related factors in adolescents and young adults with cancer. Supportive care in cancer, 31:247, 2023
2. Matsuoka H, Tsurutani J, Chiba Y, Fujita Y, Sakai K, Yoshida T, Nakura M, Sakamoto R, Makimura C, Ohtake Y, Tanaka K, Hayashi H, Takeda M, Okuno T, Takegawa N, Haratani K, Koyama A, Nishio K, Nakagawa K. Morphine Versus Oxycodone for Cancer Pain Using a Catechol-O-methyltransferase Genotype Biomarker: A Multicenter, Randomized, Open-Label, Phase III Clinical Trial (RELIEF Study). The oncologist, 28:278-e166, 2023
3. Matsuoka H. [Psycho-Oncology: An Overview of Clinical Practice Guidelines for the Care of Psychologically Distressed Bereaved Families Who Have Lost a Family Member to Physical Illness, Including Cancer]. Brain and nerve = Shinkei kenkyu no shinpo, 75:77-83, 2023
4. Hirayama T, Fujimori M, Ito Y, Ishida Y, Tsumura A, Ozawa M, Maeda N, Yamamoto K, Takita S, Mori M, Tanaka K, Horibe K, Akechi T. Feasibility and preliminary effectiveness of a psychosocial support program for adolescent and young adult cancer patients in clinical practice: a retrospective observational study. Supportive care in cancer, 31:146, 2023
5. Sadahiro R, Wada S, Matsuoka YJ, Uchitomi Y, Yamaguchi T, Sato T, Esaki M, Yoshimoto S, Daiko H, Kanemitsu Y, Kawai A, Kato T, Fujimoto H, Uezono Y, Shimizu K, Matsuoka H. Prevention of delirium with agitation by yokukansan in older adults after cancer surgery. Japanese journal of clinical oncology, 52:1276-1281, 2022
6. Ishiki H, Hasuo H, Matsuda Y, Matsuoka H, Hiramoto S, Higuchi M, Yoshida K, Tokoro A, Hatano Y, Hori T, Kinkawa J, Nojima M. Prevalence of Myofascial Pain Syndrome and Efficacy of Trigger Point Injection in Patients with Incurable Cancer: A Multicenter, Prospective Observational Study (MyCar Study). Pain medicine (Malden, Mass.), 23:1259-1265, 2022
7. Hirayama T, Fujimori M, Yanai Y, Ishiki H, Shindo A, Tanaka M, Kobayashi T, Kojima R, Satomi E. Development and evaluation of the feasibility, validity, and reliability of a screening tool for determining distress and supportive care needs of adolescents and young adults with cancer in Japan. Palliative & supportive care, 1-11, 2022
8. Terada T, Hirayama T, Sadahiro R, Wada S, Nakahara R, Matsuoka H. Pilot Study of Lemborexant for Insomnia in Cancer Patients with Delirium. Journal of palliative medicine, 25:797-801, 2022
9. Matsuoka H, Clark K, Fazekas B, Oyamada S, Brown L, Ishiki H, Matsuda Y, Hasuo H, Ariyoshi K, Lee J, Le B, Allcroft P, Kochovska S, Fujiwara N, Miyaji T, Lovell M, Agar M, Yamaguchi T, Satomi E, Iwase S, Phillips J, Koyama A, Currow DC. Phase III, international, multicentre, double-blind, dose increment, parallel-arm, randomised controlled trial of duloxetine versus pregabalin for opioid-unresponsive neuropathic cancer pain: a JORTC-PAL16 trial protocol. BMJ open, 12:e050182, 2022
10. Akechi T, Kubota Y, Ohtake Y, Setou N, Fujimori M, Takeuchi E, Kurata A, Okamura M, Hasuo H, Sakamoto R, Miyamoto S, Asai M, Shinozaki K, Onishi H, Shinomiya T, Okuyama T, Sakaguchi Y, Matsuoka H. Clinical practice guidelines for the care of psychologically distressed bereaved families who have lost members to physical illness including cancer. Japanese journal of clinical oncology, 52:650-653, 2022
